The SPH Medical RoWalker Helping Mobilize Patients
Studies show the efficacy of mobilize patients early, and its benefits contribute significantly to patient health. Everyone on a health care team shares an interprofessional responsibility to provide treatment. However, the task of delivering ambulatory care typically rests with nurses who spend more time with patients than other health care team members. The SPH Medical RoWalker assists in providing the service that patients require, and it makes delivery easier for nurses.
Considering the Benefits of Early Patient Mobility
Combating the harmful effects of immobility on deconditioned patients, early patient mobility equipment contributes significant benefits. It improves muscle strength for bed-bound patients after days of immobility and inactivity. In addition, it reduces the incidence of delirium. Patients who use it tend to achieve better functional status after hospital release. Experts point to a potentially lower rate of mortality as well.
A reduction in days on a ventilator or in the ICU helps lower the cost of hospital care. When you mobilize patients early it improves respiratory and circulatory function in ICU patients. Getting out of bed and moving around multiple times a day with the RoWalker improves health outcomes significantly. Treatment that can produce a reduced length of stay helps improve patients’ overall quality of life.
As a falls prevention and ambulation tool that mobilizes patients, the RoWalker has proven its value across the country with a 10-year record of reliability. Moreover, early patient mobility does much more than making it easier for patients to move around from one location to another. While it may not occur to others who can move about freely, mobility lets people take care of routine activities of daily life. It provides opportunities for the expression of emotions and gratification of needs that everyone experiences. As an aid to enhancing the body’s ability to repair an injury and heal itself, the RoWalker serves an invaluable purpose.
Assisting Nurses in Providing Care
Research shows that functional decline in patients accompanies immobility. Outcomes include falls, delirium, increased length of hospital stay and an inability to conduct daily activities. Additionally, the loss of ambulatory independence can affect the quality of life. Enabling patients to move about, the SPH Medical RoWalker delivers care efficiently and enhances the safety of care providers. Nurses can rely on the equipment to provide the measure of support that a patient requires. In addition, the design makes it easy for both nurses and patients to use.
Understanding the Conveniences
The design of the RoWalker incorporates the features that give patients and nurses assurance of efficiency and safety. With a 400-lb weight capacity, it mobilizes patients early and reduces the length of stay. The effectiveness of the design challenges patients to walk a little further with confidence and without the need for additional falls prevention.
Using the SPH Medical RoWalker provides the confidence and sense of well-being that encourages deconditioned patients with muscle weakness from inactivity to use it. Nurses can facilitate progress without strain or worry as the equipment handles every challenge smoothly and efficiently.
- Movement Control
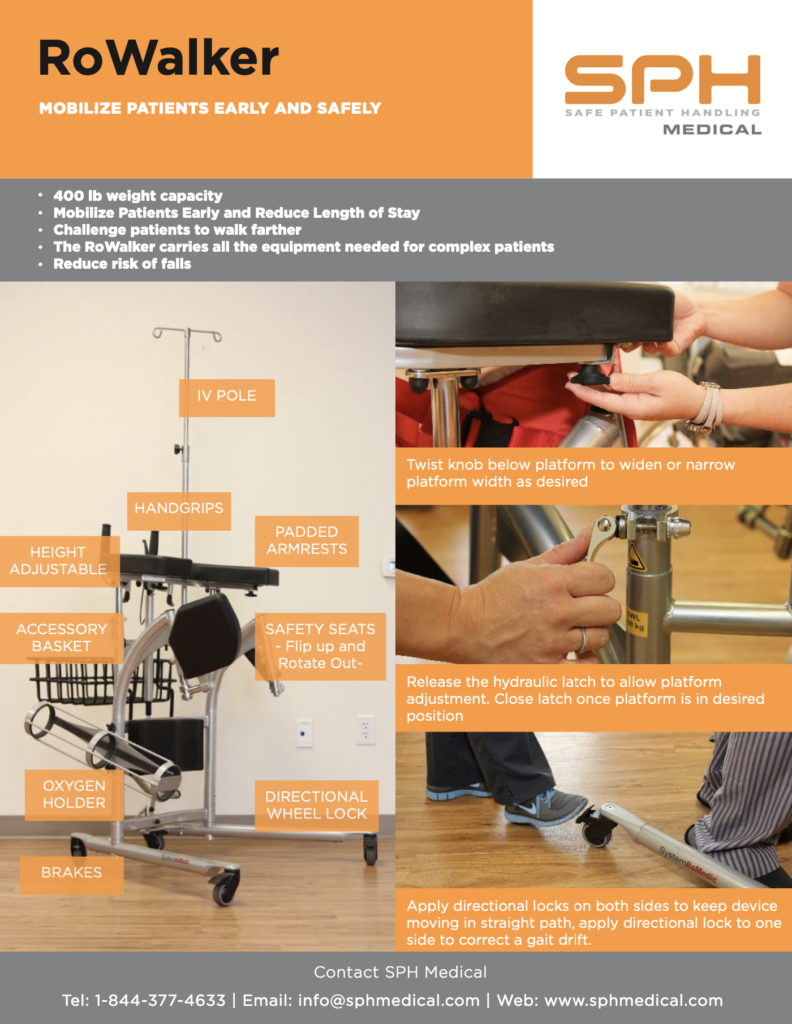
Brakes and a directional wheel lock feature control the movement of the RoWalker. The directional locks enable the SPH Medical RoWalker to track in a straight line. Conveniently located and easy to access, the brakes and locks provide safe and reliable ambulation. - Access to Oxygen
An oxygen tank holder with a convenient location on the front of the RoWalker ensures access to oxygen for patients when needed. - Seating Comfort and falls prevention
Seats can flip up and rotate out to make it easy for patients to get into position to use the equipment. The seat flaps allow a patient to take a rest and sit down if they get tired. The seat flaps eliminate the requirement to pull a wheelchair behind a patient to try to catch a falling patient. Padded armrests and hand grips provide the extra comfort level that encourages patients to get the exercise that early patient mobility offers. - Height Accommodation
An adjustable height feature allows the SPH Medical RoWalker to serve patients of any size. The equipment adapts to the height of each patient instead of requiring nurses to provide alternative measures. An adjustable IV pole stands above the unit to allow unimpeded access to the vital supply that patients may need while getting ambulatory exercise. - Storage Basket
On the front of the RoWalker, an attractive metal basket provides a convenient place to store cardiac monitors or other small items that patients may need while away from their room.
Choosing Effective Equipment to Mobilize Patients
Years of development based on feedback from respiratory and physical therapists, nurses and cardiothoracic surgeons have produced the unique ergonomic design of the SPH Medical RoWalker. Initially designed for post cardiac/abdominal surgery patients, it has become the preferred choice for early patient mobility. In addition, major departments in hospitals across the country choose it for complex patient conditions, falls prevention and encouragement to exercise safely.