Epidurals have transformed pain management during labor, offering significant relief to millions of mothers worldwide. However, administering an epidural is a precise and delicate process that relies heavily on proper patient positioning. Discomfort, instability, and improper alignment can result in complications or a prolonged procedure. This is where the Epidural Positioning Device (EPD), also known as the Epidural Positioning Chair, plays a vital role. Designed to improve both patient and staff experience, the EPD is setting new standards for efficiency, comfort, and safety in labor and delivery units.
Features and Benefits of the EPD for Nursing Staff
Labor and delivery nurses face constant physical demands in their fast-paced work environment. The EPD is an innovative solution engineered to reduce stress and improve workflow. Its ergonomic design minimizes the physical strain associated with positioning laboring mothers for epidural administration.
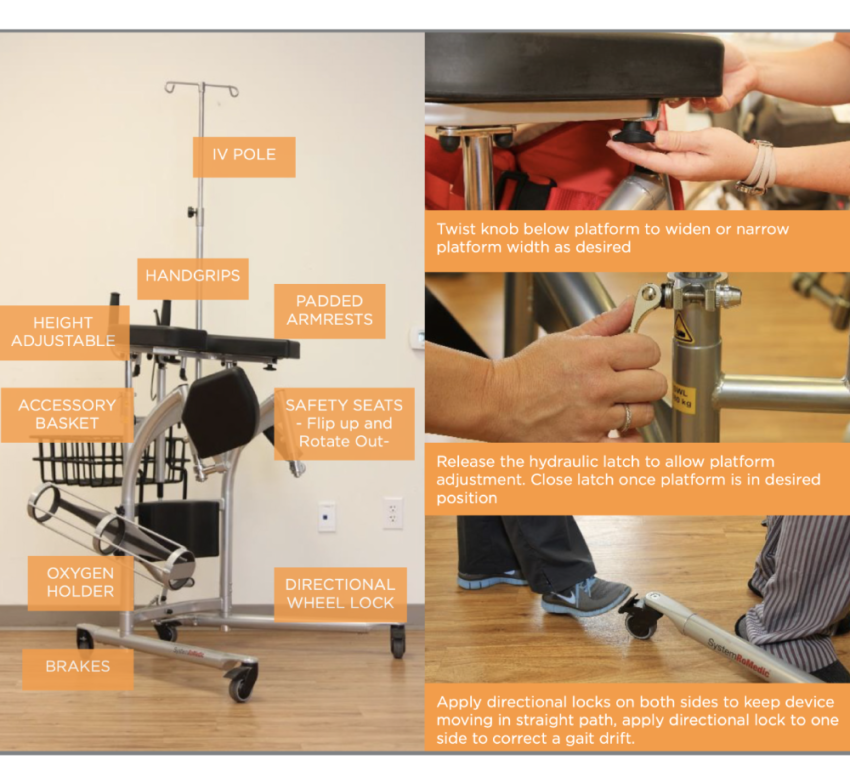
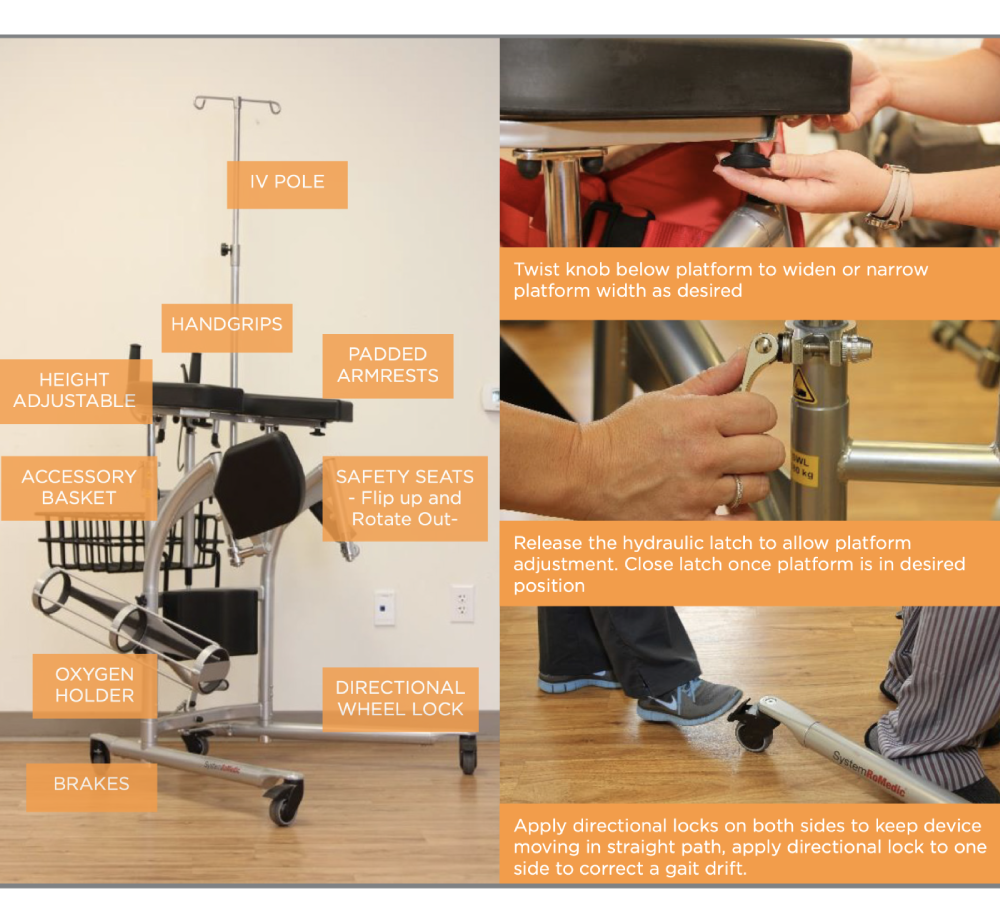
Key features like adjustable height and stepless chest cushion adjustments ensure that nurses can adapt the positioning to each patient’s unique anatomy, even during hectic situations. These flexible adjustments considerably reduce the need for manual lifting or holding, which are common causes of musculoskeletal injuries among nursing staff. Additionally, the EPD helps ensure standardization and consistency across procedures, giving nurses confidence in their equipment and freeing them to focus on patient care.
How the EPD Improves Patient Safety and Comfort
Patient safety and comfort are paramount during labor and delivery, especially during epidurals. The EPD offers unparalleled support to expectant mothers, ensuring proper spinal alignment and reducing unnecessary movement during the administration process. This stability directly contributes to improved accuracy, which can minimize complications such as inadequate analgesia or nerve injuries.
Beyond safety, the EPD also prioritizes maternal comfort. Its padded chest cushion, face rest cushion, and adjustable armrests provide a secure and relaxed experience, even for mothers undergoing intense labor pains. Knowing they are stable and well-supported can ease some of the anxiety that often accompanies medical procedures, helping mothers focus on their labor and delivery process. A more comfortable and relaxed patient is often more cooperative, which can speed up the epidural process and reduce overall stress for both the mother and the medical team.
Impact on Staff Efficiency and Safety
When hospitals prioritize the health and safety of their staff, patient care improves across the board. The EPD contributes significantly to operational efficiency in labor and delivery units. Its user-friendly design eliminates the need for makeshift supports like pillows or manual assistance from extra staff members. This not only shortens epidural procedure times but also optimizes the workflow, especially when handling multiple laboring mothers simultaneously.
The EPD also significantly reduces the risk of injuries for staff, which is crucial in maintaining a healthy workforce. Musculoskeletal injuries are a leading cause of absenteeism among nurses, with improper patient handling being a major culprit. By alleviating the physical demands of positioning, the EPD enhances workplace safety, reduces burnout, and allows medical teams to focus on what matters most—providing excellent care to mothers and their newborns.
Real-World Impact
Hospitals already using the EPD in their labor and delivery departments have seen measurable improvements in staff safety. Nursing staff report reduced fatigue during long shifts, thanks to the device’s ergonomic design, while feedback from laboring mothers highlights the chair’s ability to provide much-needed comfort during a challenging process.
One labor and delivery unit noted a 20% reduction in epidural procedure times after implementing the EPD. An L&D manager from a high-volume hospital shared, “The EPD has been a game-changer for our team. It’s not just about safety—it’s about the experience we create for mothers and staff alike. We’ve seen fewer injuries and happier patients since we started using it.”
The Epidural Positioning Device is revolutionizing labor and delivery departments by enhancing comfort, safety, and efficiency during epidural procedures. Its unique features reduce physical strain on nursing staff, promote maternal safety, and improve procedural accuracy. As hospitals look for ways to elevate patient care and protect their staff, adopting the EPD represents a step forward in achieving these goals.
Hospitals that invest in innovative tools like the EPD pave the way for improved outcomes and higher satisfaction rates for both patients and their healthcare teams. It’s not just an investment in equipment, it’s an investment in better, safer, and more compassionate care.