When undergoing medical procedures, the safety of patients and medical staff alike is of utmost importance. This is especially true when a patient is at increased risk due to surgical intervention or other complex procedures that could lead to severe injuries or additional health complications. As such, risk reduction during Thoracentesis must be employed to safeguard all parties involved. Case in point, an epidural positioning device, or EPD, is utilized for those undergoing thoracentesis procedures.
The Importance of an EPD and How It Works
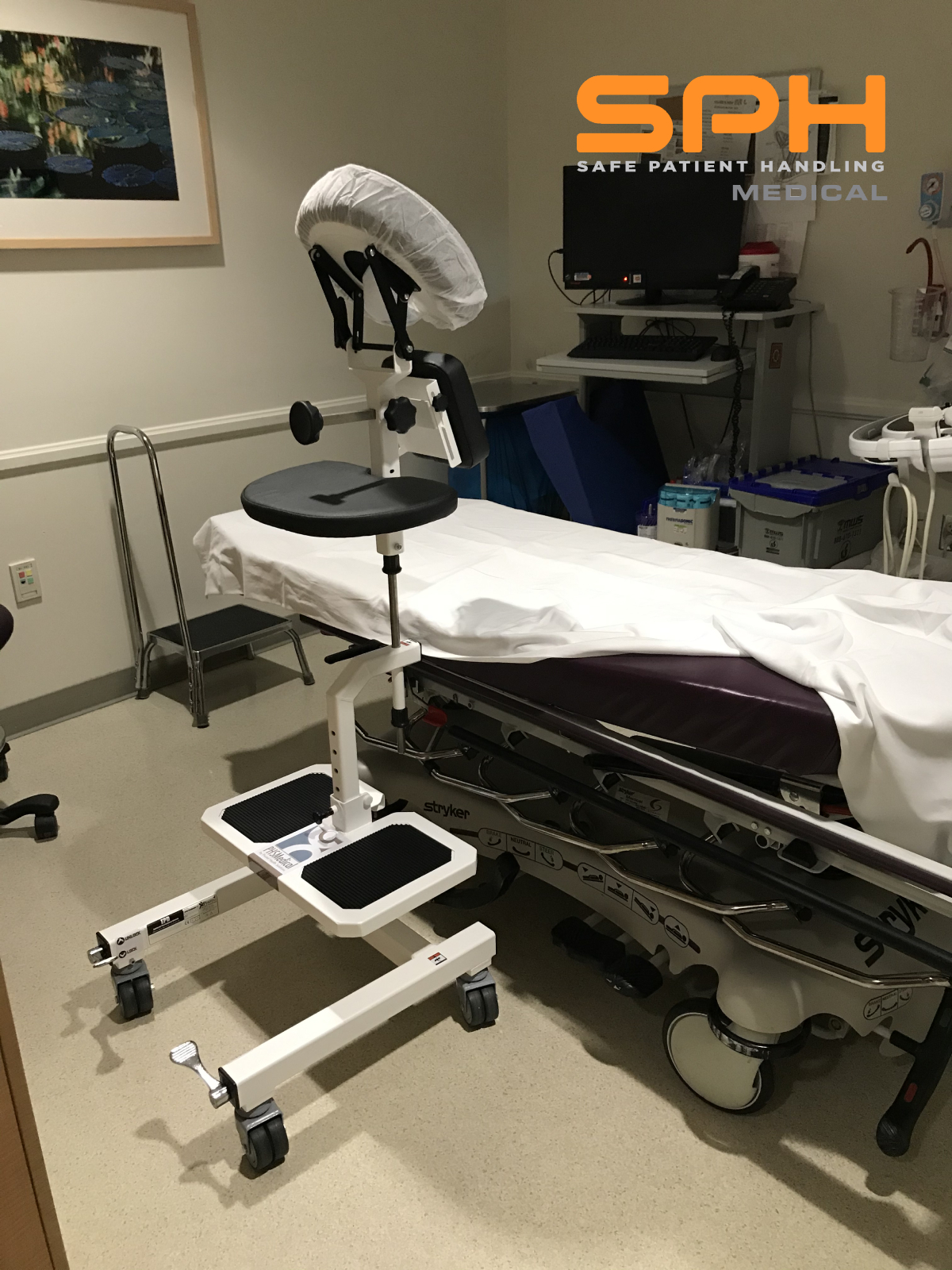
The use of an epidural positioner, which is more commonly known as an epidural chair, has become the standard of care when it comes to securely positioning of individuals in peri-operative areas preparing for surgery and spinal blocks or in diagnostic imaging areas where ultrasound technicians are preparing patients for Thoracentesis. Moreover, this tool also helps reduce the risk of nursing injury and potential harm to other caregivers. Originally developed more than 20 years ago for obstetrics, pre-op, and spinal procedures, its use allows for the proper positioning of patients during a spinal block, epidural placements, land a myriad of medical procedures. Moreover, it touts many benefits for users and caregivers alike.
Epidural positioners assist with lumbar, thoracic, and cervical flexion while ensuring proper alignment and bolstering stability. There are two types of EPDs, one manual or non-powered, and one electric. The manual version features a spring-loaded adjustment control that operates the midsection and footrest portions. Meanwhile, the electronic version, or e-EPD, operates via motorized control of the midsection and footrest. EPDs are commonly found in hospitals, pain management clinics, surgical suites as well as labor and delivery rooms. Moreover, they are an ideal support device for thoracentesis, obese, and OB/GYN patients.
Understanding the Thoracentesis Process And Risk Reduction During Thoracentesis
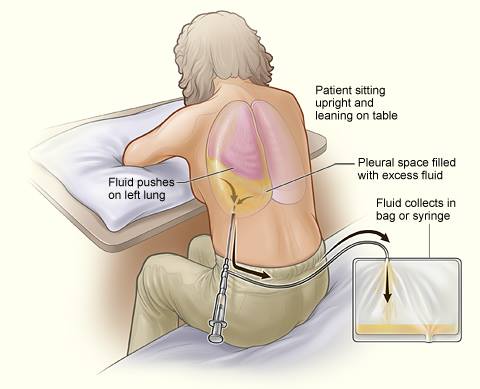
 During this procedure, technical staff are charged with positioning the patient in a comfortable upright position to enable the Doctor to extract fluid from the pleural cavity, which is situated between the lungs. This is accomplished via the insertion of a small needle through the chest wall and into the plural cavity to drain the fluid and is typically performed by a Doctor or Pulmonologist. The EPD device has an adjustable footplate, chest support, armrests, and a headrest for risk reduction during Thoracentesis and to ensure the proper positioning as well as comfortable placement of the user. These features work together to not only provide support and comfort, but the device significantly bolsters patient safety, improves patient comfort, and minimizes the risk of patient falls while significantly safety for the medical staff during Thoracentesis, epidurals, spinal blocks or other spinal procedures.
During this procedure, technical staff are charged with positioning the patient in a comfortable upright position to enable the Doctor to extract fluid from the pleural cavity, which is situated between the lungs. This is accomplished via the insertion of a small needle through the chest wall and into the plural cavity to drain the fluid and is typically performed by a Doctor or Pulmonologist. The EPD device has an adjustable footplate, chest support, armrests, and a headrest for risk reduction during Thoracentesis and to ensure the proper positioning as well as comfortable placement of the user. These features work together to not only provide support and comfort, but the device significantly bolsters patient safety, improves patient comfort, and minimizes the risk of patient falls while significantly safety for the medical staff during Thoracentesis, epidurals, spinal blocks or other spinal procedures.
In summary, an epidural chair is a useful tool that provides comfort and stability for individuals undergoing various medical procedures, such as spinal blocks, epidurals, Thora’s, and other spinal issues that require flexed spine positioning for ideal needle placement. More importantly, an EPD facilitates a combination of safe patient handling, optimal positioning, minimizes the risk of complications, and reduces the likelihood of injury to patients as well as caregivers alike.