Nurses Are Becoming Increasingly At Risk For Workplace Injuries
Now more than ever, there is a shortage of nurses. Many older nurses are hitting retirement age, and the COVID virus Pandemic has not been kind to these figures either. More nurses are needed, and fewer are available. This issue is correlating unfortunately well with other directly related topics. Patients are getting much heavier, and States are legislating to mandate safety programs in hospitals. These programs are not a negative factor, but in regards to fewer nurses and more serious patients, more and more injuries are occurring for nurses in the workplace. Nurses are in the top three professions at risk for receiving Musculoskeletal Injuries that are potentially career-ending. The overall objective is safe patient handling while simultaneously minimizing workplace injuries. If nurses could move larger patients without risking injury, it would benefit the nursing shortage as well. Also, if a larger patient is coding, time is a crucial resource. If a nurse doesn’t have to struggle to reposition or transfer a patient, it can potentially be life-saving. This is where the SPH Medical Air Transfer Systems can help save time and resources in a critical situation.
Other Technologies Have Been Used But Remain Limited
There have been other systems and technologies in place. Ceiling lifts were installed in newer hospitals and were retrofitted in several older hospitals. The main concern with this system is mobility. Ceiling lifts are attached to a permanently mounted track that positions a patient inside of a sling. Mobile lifts solve that issue with wheels. They can be very cost-effective, but typically two careers are required when hoisting a patient.
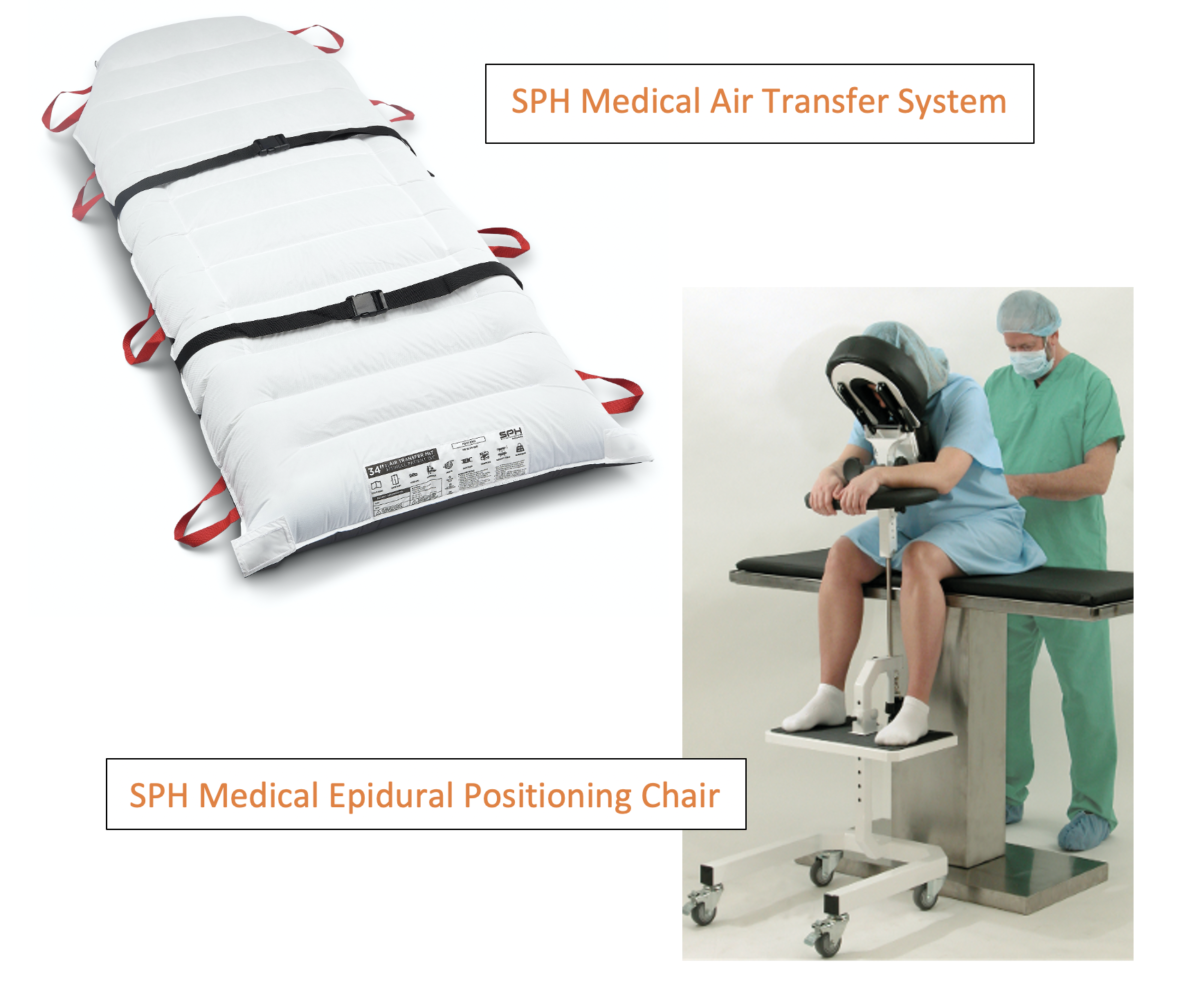
Air Assisted Transfer System
The Air Assisted Transfer System or sometimes referred to as an Air Powered Transfer System, is the preferred technology with nurses. Minimal effort is needed when using these systems to move patients. From bed to gurney, a bed to OR Tables, a bed to x-ray or CT table, the Air-Powered Transfer System is a multifaceted solution. They are highly portable and can be moved with a patient as they are relocated on a stretcher or bed.
How Air Transfer Systems Works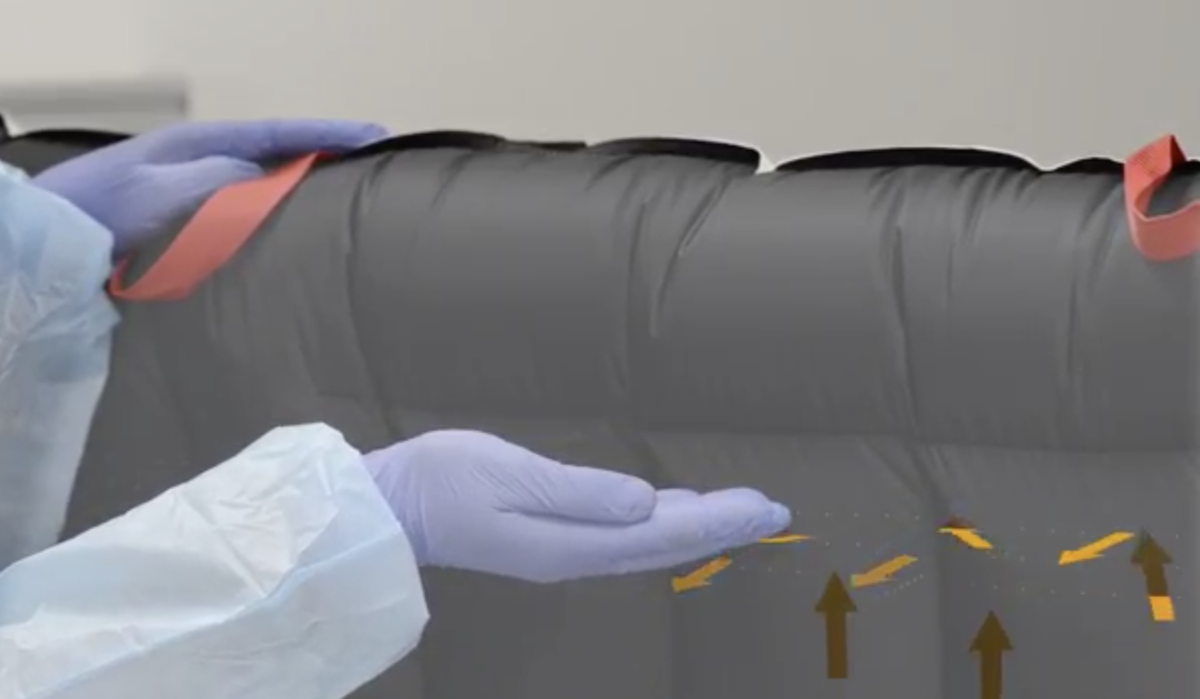
After the patient is securely placed on the mattress, low-pressure air pushed from an air supply will inflate the breathable transfer mattress. The air supply supports the patient comfortably and air escapes perforations in the bottom of the mattress supporting the mattress on a mobile bed of air. This reduces friction and facilitates near-effortless patient transfers. This, in turn, results in caregivers using a significant decrease in physical effort. The air patient transfer system decreases exertion and meets workplace safety guidelines.
The Benefits Push Beyond Mobility And Required Exertion
With a Single Patient Use Transfer Mattress System, there are benefits beyond eliminating injuries within the workspace. Air-assisted technology moves patients with more stability. This, in turn, reduces skin shearing and bruising during transfers. Single Patient Use Air Transfer System also eliminates costs and logistical issues that are associated with reprocessing. During typical situations, this reduces the risk of cross-contamination. During a pandemic like COVID, the benefits exceed even greater. The air-assisted technologies are also MRI compatible and vary style and width, and can accommodate patients that weigh 1000lbs.
Air Transfer Systems Can Be used Anywhere
These systems can be used in any hospital department. This is extremely useful where transfers are common and are a daily occurrence. There are also particular departments where ceiling lifts are too challenging to install. The ICU, MedSurgery, OR, Imaging Department, Transport, and Emergency Rooms are all sectors that could yield massive results from implementing these technologies. Essentially, ANYWHERE lateral patient transfers are made from one surface to another, or frequent repositions are made can benefit from their usage.
The Multifaceted Benefits from Using Air Assisted Transfer Systems are Too Great
The results speak for themselves. Right now, this is the premier equipment in safe patient handling. These technologies are an extra pair of hands for our quickly dwindling nurse workforce, allowing more effective utilization of human resources within the bounds of the hospitals. It is also an extra measure of safety, assuring the crew isn’t taking unnecessary risks and potentially receiving musculoskeletal injuries furthering the nursing shortage. This also reduces the direct and indirect cost of these injuries, freeing up hospital budgets thousands to millions of dollars.
They also coincide with the new safety programs being required for hospitals
Other technologies like overhead lifts, mobile lifts, slider boards, and rollerboards have seen their usage, and it is time to move past these outdated technologies. They are particular and are less of an across-the-board solution. The Single Patient Use Transfer Mattress is the best solution for the nurse, the patient, and the hospital for safety, cost-effectiveness. It could make an immediate impact on the various issues surrounding the health care scene.