Did you know hospitals administer tens of millions of epidurals and spinal blocks each year for pain relief? Most providers perform these procedures quickly, efficiently, and with the assurance that their patients are in expert hands. Sometimes, when administering anesthesia for pain relief at the hospital, the staff administering the epidural or spinal block are the victims. Safety measures are essential to protect healthcare staff members from becoming victims of their patients. To avoid nursing injury and staff accidents, medical facilities are now implementing additional safety measures, such as using an epidural positioning device, training, and safety equipment to help reduce the risk of injuries.
What is an Epidural Positioning Device (EPD)
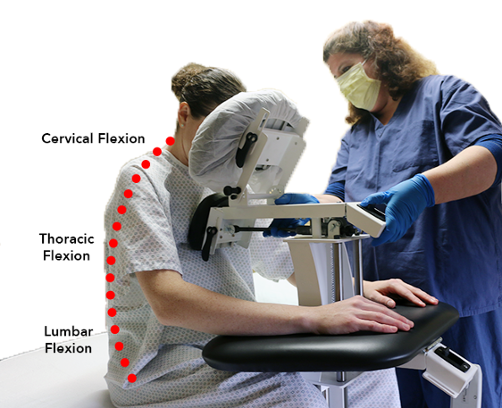
An epidural positioner is a positioning device that helps the patient lean forward into a proper position to receive an epidural while fully supported. It is known as an epidural chair and it consists of an adjustable headrest, chest pad, arm supports, and footrest. These components work together to provide stability and comfort to the patient. Epidural Positioner can reduce injuries and increase patient safety during epidurals and other anesthetic procedures. Devices like this are useful in operating rooms, labor, and pain management centers. The EPDs reduce patients’ and staff’s risk and improve safety by assisting with thoracic, cervical, and lumbar flexion while maintaining stability. EPDs are available in both manual and electric versions. The manual version has a spring-loaded knob for adjusting the midsection and footrest. An electronic controller controls the midsection and footrest in the electric version. EPDs are the best choice for obstetrics, thoracentesis, and obese patients.
What is Thoracentesis?
In this procedure, doctors remove fluid from between the lungs. With the EPDs, the headrest, armrests, and footplate are adjustable for safe and comfortable positioning for the patient. Using EPD for thora’ provides a solution to staff concerns about using the unsafe bedside table. Currently, EPDs for Thoracentesis procedures are becoming the new standard for care.
COVID-19 and the Epidural Positioning Device Use
As COVID-19 spreads, health care providers will continue to suffer disproportionately. Numerous frontline caregivers have been exposed in the U.S. to date. Manual patient handling is put into a new perspective regarding patient and staff safety, including staff distance and behavior. The manual handling of patients exposes nurses to musculoskeletal injuries and can increase their exposure to COVID-19. During spinal blocks and epidurals, the staff must hold the patients in position, increasing the risk of spreading the virus. So unnecessary contact is crucial for protecting the patient and nursing injury and sickness.
Safe Patient Handling and Epidural Positioner
Epidural and spinal blocks are techniques for perioperative pain management with multiple applications in anesthesiology. An epidural injects anesthesia into the epidural space, and a spinal block injects anesthesia into the dural sac that contains the cerebrospinal fluid. It gives immediate relief due to direct access. An epidural is a standard procedure performed during labor and delivery. Although it is useful as a primary anesthetic, its most common application is pain management. It can be a single shot or a continuous infusion for long-term pain relief. Although they are generally safe, there is always a risk of injury to the person administering the medication. Using these medications safely requires that staff be properly trained and equipped.
Safety equipment:
Staff members should use safety equipment when administering epidurals and spinal blocks. This includes gloves, goggles, and masks to protect them from potential infections and other risks and ensure their safety and the safety of the patients.
Training:
Medical staff should receive proper training in safely administering spinal blocks and epidurals. This training should include both classroom instruction and hands-on training, and it should cover the equipment needed, its setup, potential problems, and how to handle emergencies. Staff should also be physically fit. Safely performing these procedures requires physical fitness, precision, and agility. Personnel who are physically fit are less likely to suffer injuries when performing medical procedures.
Epidural Positioning Device and The Proper Technique:
Proper techniques help reduce complications and ensure that patients receive the best possible care. To administer epidurals and spinal blocks safely, staff must know most of the procedures. The epidural chair facilitates positioning. However, there are other traditional methods like the ‘mad cat position’ whereby: – The patient sits on the bed edge or lies on their side on the table or bed – A nurse stacks pillows on an unstable bedside table – The patient leans over it – A nurse places a stool under the patient’s feet In this traditional method, the nurse held the patient in the proper position during the procedure.
Documentation:
The staff should document all procedures, including epidurals and spinal blocks. The documentation can help to identify any potential problems.
Conclusion
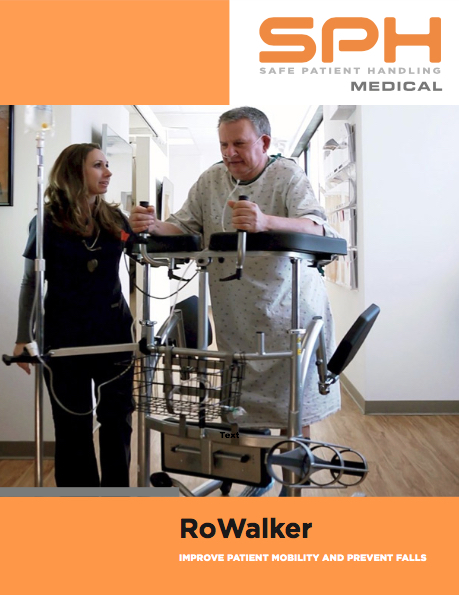
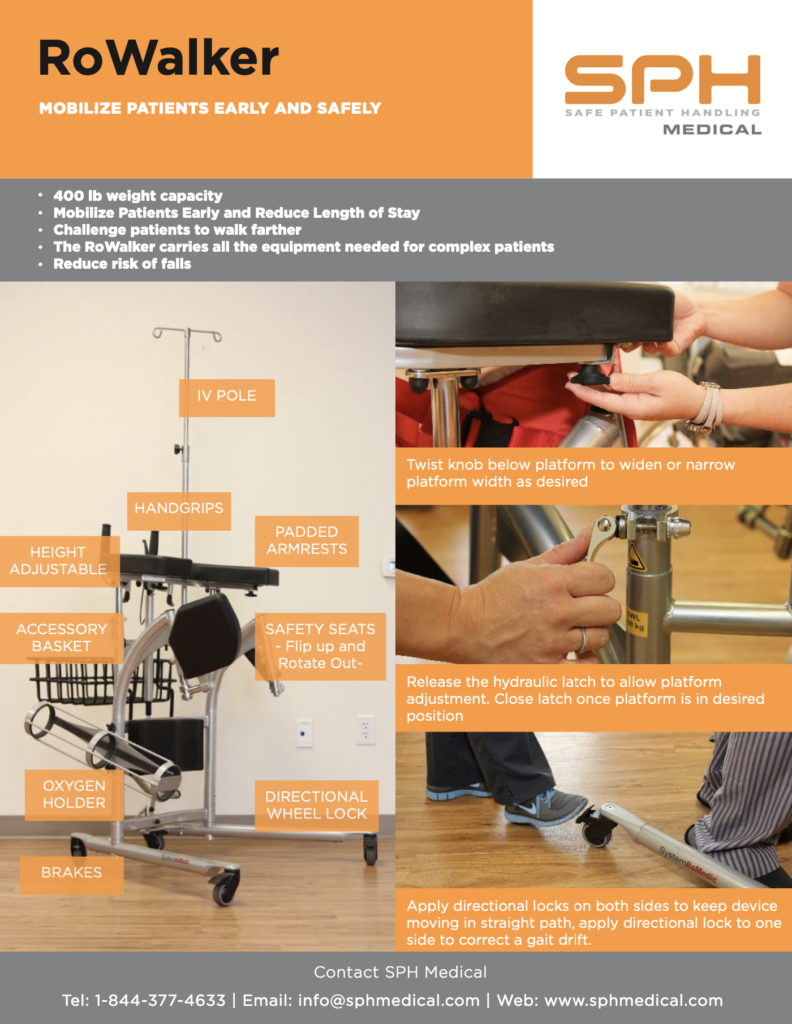
A successful mobility program and safe patient handling hinge on buying in, acquiring the right equipment, and providing guidance on the best solutions to improve patient and staff safety. Ultimately, best practices are the key. It only takes one wrong lift to ruin a nurse’s career. It takes only one snap decision to end a nursing career, and we need all our nurses.