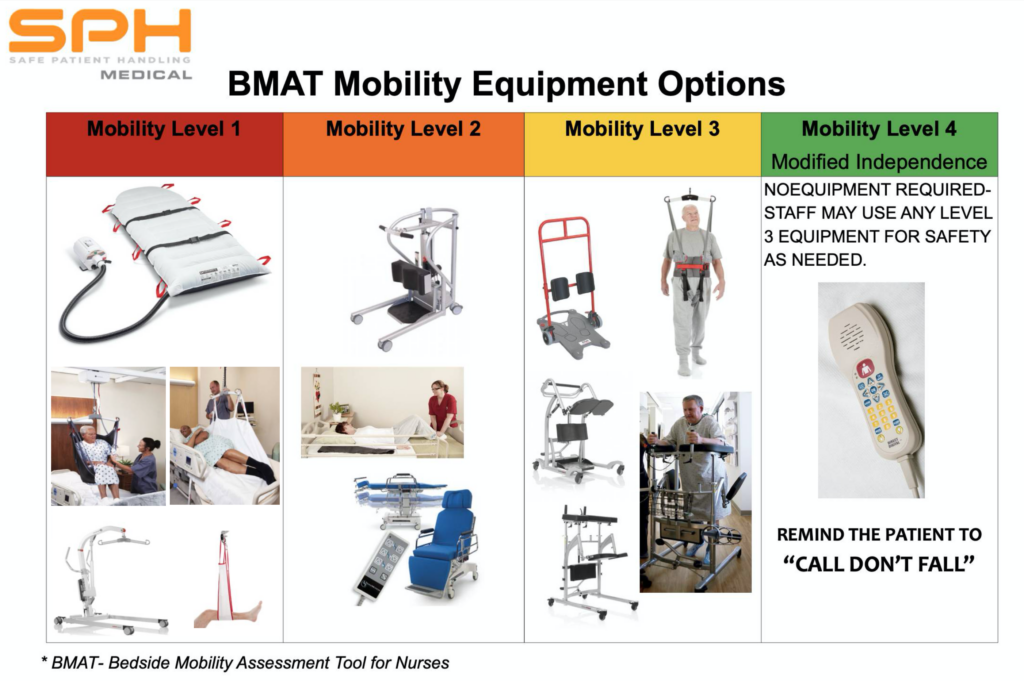
Today, Safe Patient Mobility means something different to every department in the hospital. But in general it means that we need to understand how patients move and how to safely handle them based upon their functional abilities. An important component is choosing the right assistive solution for each patient. There are a couple of tools now available that help assess a patient’s functional ability and then translate the results of that assessment to an assistive device recommendation. The first validated functional assessment tool of this kind for safe patient handling is the BMAT. We’ll go into greater detail about the history of the BMAT in another article but suffice it to say that nurses need to select use the right assistive tool based upon their functional ability to then mobilize our patients safely while maximizing the patients’ ability to move! The BMAT helps define the right tool. This article will focus on one of the highest frequency tasks that we see in hospitals today where a patient is totally dependent upon the hospital staff to be moved either up in bed or over to another surface laterally.
Safe Patient Mobility for Lateral Movement
A significant obstacle to providing therapeutic and safe environments of care is the practice handling patients manually. Sliding, lifting, positioning, and transferring patients without using assistive technology remains common in healthcare facilities. Notwithstanding, it is an unsafe practice for both patients and caregivers. Manual handling places caregivers at significant risk for nursing injury.
Scholars have established that more than eighty percent of caregivers’ work-related injuries result from a lack of safer ways to move or lift patients manually.
The increasing rate of morbidly obese, sicker, and predictable bariatric surgery patients that need to be moved around for multiple caregiving tasks amplifies the level of stress placed on caregivers’ bodies. It calls for some little imagination to understand that the nursing injury impacts organizational and staffing costs associated with workers’ compensation, lost time, and, most importantly, the quality of care. At the same time, manual patient handling increases the risk of pain, repositioning injury, and adverse health outcomes.
Risk Of Injury
According to research, of all professional groups, healthcare has the most significant number of work-related injuries. Globally, 50 to 60 percent of healthcare professionals are suffering from muscular-skeletal disorders. Repositioning, lateral transfer and movement are the most cited patient handling tasks in clinical facilities, and if performed manually, they endanger both patient and staff health. The air-assisted transfer system, such as the SPH Medical Air Transfer System, presents a practical approach to mitigating repositioning injury risks and physical effort related to the performance of transfers while reducing healthcare costs and work-related injuries. It allows the release of low-pressure air via the perforated chambers within its transfer mattress. The system creates a thin air cushion under an inflated mattress to lower friction and protect the patient’s skin, leading to improved care and injury risk reduction.
Cost Implications
According to International Labor Organization (ILO), the economic impact of not investing in health and worker safety is approximately equal to the collective gross domestic product of the one hundred and thirty poorest nations globally. The organization revealed that 2.78 million workers die annually due to occupational illnesses and injuries. An estimated 2.4 million of these deaths are associated with work-related illnesses. The annual aggregate cost of these injuries, diseases, and deaths is $2.99 trillion or approximately 4% of global GDP. There is a worldwide recognition that some OSHA challenges require global solutions.
Legislation
The HGRC Specialty Subcommittee on Patient Movement has studied the application of patient movement and handling equipment within health facilities. In sharing its expertise and research, ILO shockingly established a lack of information and knowledge on the issue and a growing recognition among regulatory agencies and the healthcare industry of the need to address this concern. The healthcare industry, nurses labor unions, nurses’ associations, state and federal regulators, and state legislatures have argued in favor of the capital costs associated with bills mandating minimal lift policies and the adoption of Air Transfer Systems to mitigate caregiver injuries.
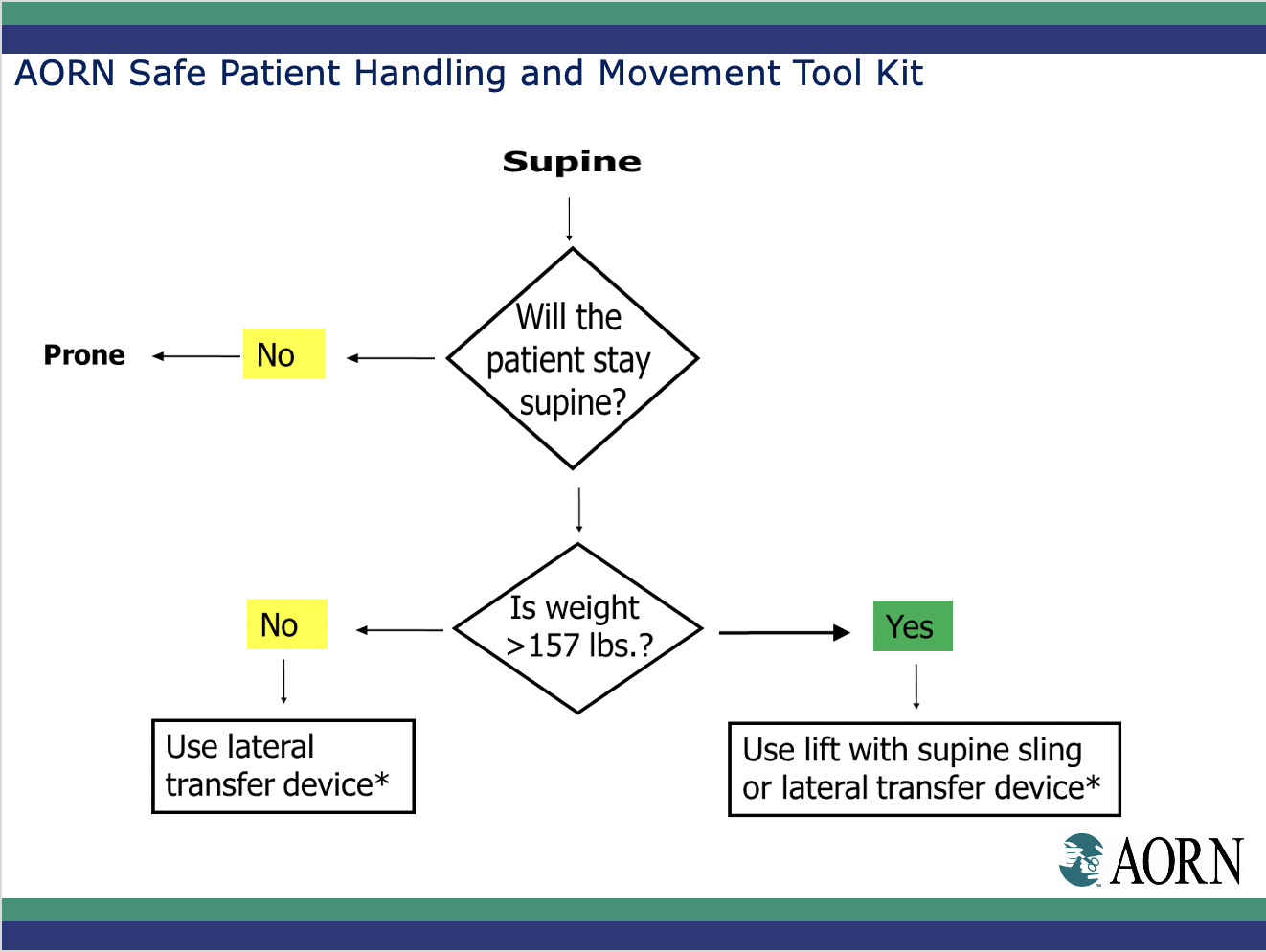
Several states have enacted patient handling resolutions or legislation. Moreover, Washington and Minnesota have committed funds for loan or grant programs to help acquire these devices. American Nurses Association (ANA) standards on Safe Patient Handling and Mobility (SPHM) recommend that healthcare facilities focus on establishing a culture of safety, adopting and implementing the SPHM program, and installing and maintaining SPHM technology. Similarly, the Association of periOperative Registered Nurses (AORN) and Occupational Safety and Health Administration (OSHA) also recommends the use of lateral sliding to aid lateral transfer to support patient movement and repositioning.
Benefits
The benefits accrued from the Air Transfer devices include the following:
- They enhance the quality of life for both caregivers and patients and better patient outcomes.

- There are multiple economic benefits that are enormous, especially those associated with cost implications for direct medical expenses incurred due to injury, lost time, and workers’ compensation.
- They address the top two high risk tasks that cause injury to nurses, repositioning and lateral transfers.
- They assist in the transfer of patients with exceedingly less exertion, keeping patients well-positioned and comfortable.
- The Single Patient Use design of the Air Transfer Mattress supports the hospitals infection prevention program and significantly reduces the risk of cross-contaminating other patients or surfaces with deadly pathogens.
- The SPH Medical Air Transfer System addresses all lateral transfer needs in Surgery, ICU, Medical floors, imaging and in Labor and Delivery units.
- Air Transfer Systems also assist transport staff and all departments to promote workplace efficiency by improving patient throughput while reducing risk of injury.
Integrating air-powered transfer and positioning solutions will benefit staff, patients, and the entire industry through improving efficiencies, reducing costs, and will fundamentally improve patient satisfaction and care.
Contact SPH Medical to discuss implementing evidence based safe patient mobility solutions in your facility or department.