The use of the EPD for patient positioning during spinal blocks and other procedures
To assist in enhancing patient and staff safety, a distinguished anesthesiologist created the first Epidural Positioning Device (EPD) over two decades ago. The EPD is currently the gold standard for positioning devices used by hospital’s surgery department and surgical personnel all around the globe.
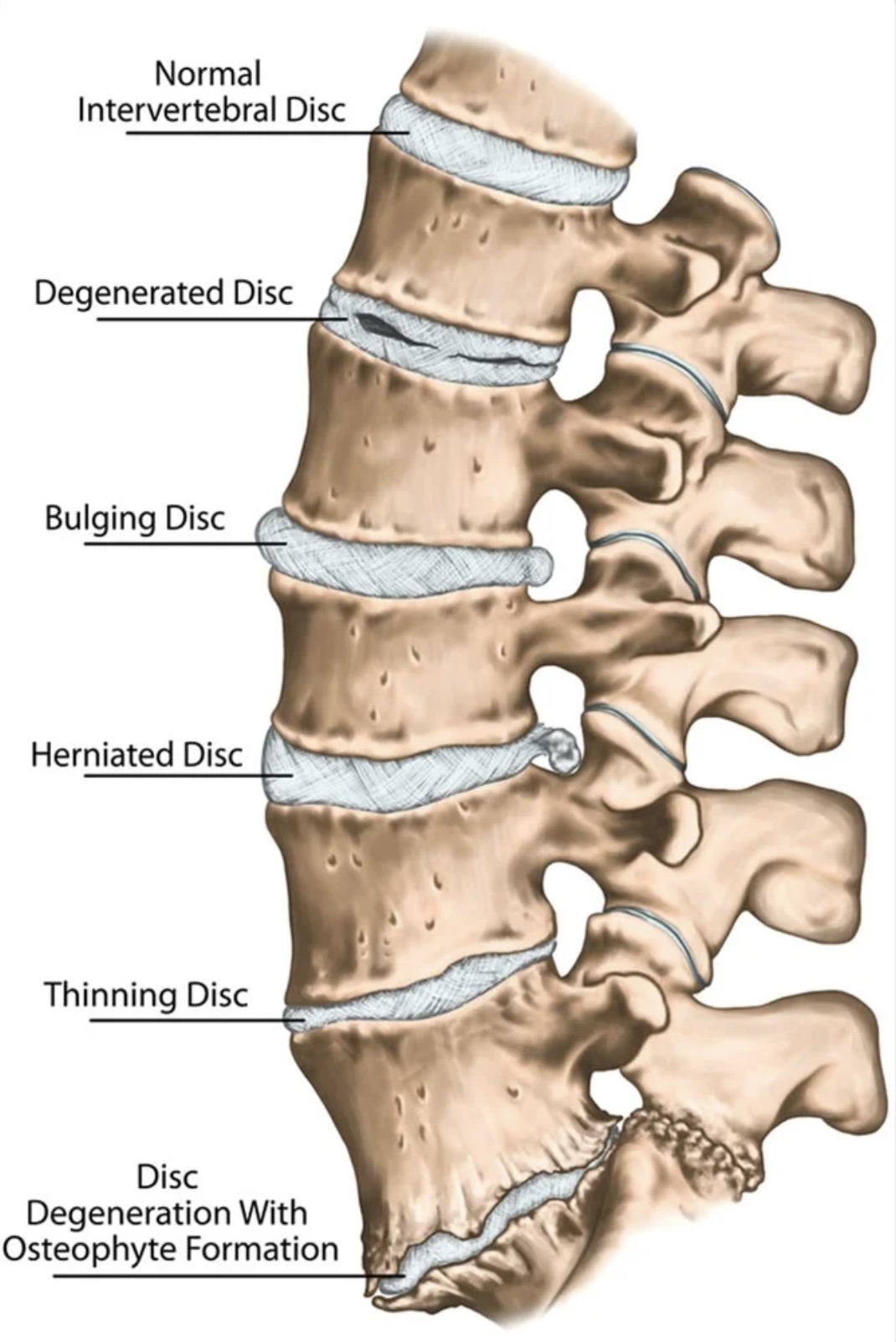
The epidural device aids in the safe positioning of patients while also lowering the risk of musculoskeletal disorders to healthcare workers. The epidural chair is most often used to position a patient for an epidural placement. Still, it is effective in situating patients securely for a range of medical procedures by promoting optimal lumbar, thoracic, and cervical flexion, offering several advantages for both patients and caregivers.
Manually moving and positioning patients for an epidural is usually done by having a patient lean over an unstable bedside table, stacked with pillows and a chair or stool to support their feet. A nurse or nurse assistant would first position the patient at the side of the bed or table, place their feet on a chair or stool, then bring over the bedside table that doesn’t lock, and stack pillows on the table so the patient can lean forward on the pillows. This approach is insecure and unstable since the table could move, pillows may easily slip out of place, and the set height of the chair or stool is inconvenient for certain people. The nurse is challenged to hold onto the patient and the table so nothing moves.
On the other hand, the EPD, or Epidural Chair as it often known, has a stable lockable base. It’s adjustable to accommodate patients of all sizes. The vertical height adjustment, foot platforms, arm rests, and face rest cushion allow each patient to be placed in the most comfortable position possible for the treatment. The chest cushion promotes the optimal spinal flexion. Now with the use of the EPD the patient is in a secure and safe position to avoid any movement during needle insertion,
In the past the nurse or nursing assistant would often maintain the patient’s position while supporting part of their body weight. To make matters worse, patients are anxious, unpredictable, often in pain, occasionally drugged, and may move unexpectedly, placing the nurse in danger. These extended static holds, and counter pressure tasks have been highlighted as high risk by leading hospital ergonomic teams, who have tried to rethink the Epidural and Spinal Block Placement procedures to eliminate the manual patient handling components due to the predictable nature of daily routine. The positioning device was created to address these concerns.
Benefits of the Epidural Positioning Device
- Mitigates Risk of Complications
There is a considerable risk of complication due to the patients’ sudden movement during spinal blocks and epidural treatments. Caregivers have been using their body and manual handling to keep the patient in the proper position for these procedures which is often unstable. Patients are prone to moving involuntarily during the procedure which may lead to inaccurate needle placement. A solid ergonomic positioning option such as the epidural positioning device provides the spinal flexion needed and the stability required to provide a smooth and accurate procedure. - Eliminates Risk of Injury
Nurses and caregivers physically position patients for epidural placements in labor and delivery units all day, every day. Nurses also prepare patients for Spinal Blocks in preoperative settings and operating rooms. Sonographers, or ultrasound techs, are also positioning patients in the imaging department for Thoracentesis. In most cases, the caregiver must use their arms and body to maintain a steady grip on the table, stool, and patient during the treatment.
Assisting the patient in maintaining a flexed spinal posture puts the nurse or helper in danger of suffering a musculoskeletal injury. Hospital ergonomic experts have documented that repetitive static holds, especially with awkward body posture, may also lead to injury. This old fashioned way of doing things has resulted in predictable strains, sprains, and workplace injuries. The EPD solves these issues and provides a standardized and efficient process that improves nursing and caregiver safety while avoiding the high risk tasks of manually holding and supporting the patient.
Improves Patient’s Comfort and Satisfaction
According to recent research, patient comfort was greatly improved when the EPD was used instead of flexion alone for pregnant women having an epidural. It was also discovered that needle placement would be easier if the patient was more comfortable.
Labor and delivery unit, general surgery, operating rooms, anesthesia, radiology, and pain management clinics are all places where EPDs are now standard. Epidurals, spinal blocks, and thoracentesis procedures are all performed using the EPD. Every medical institution must make every effort to keep patients safe and comfortable while preventing harm to nurses. EPDs put patients in the best possible position to enable the anesthesiologist to do their best work. The Epidural Chair helps keep patients in position while the needle placement occurs by creating a solid, stable, and pleasant environment.
The device was developed to provide ideal spinal flexion and access to the lumbar, thoracic and cervical areas, but it has recently gained popularity for supporting patients during thoracentesis procedures. The imaging department is generally involved with “thora’s” as they prepare the patient and locate the ideal spot on the rib cage to prepare for the treatment. They have also been using the unstable bedside table for positioning and a stool. Now with the EPD patients are easily positioned in a comfortable position to enable the pulmonologist to insert the catheter to drain excess fluid from the pleural space.
Patients benefit from the secure feeling and comfort provided by the epidural patient positioning device. When the patient is properly positioned with the EPD, the caregiver doesn’t have to rely on their arms, shoulders, and hands to keep them in the best posture for the treatment. These advantages significantly minimize the risk of staff injuries and complications during epidurals, spinal blocks and thora’s.