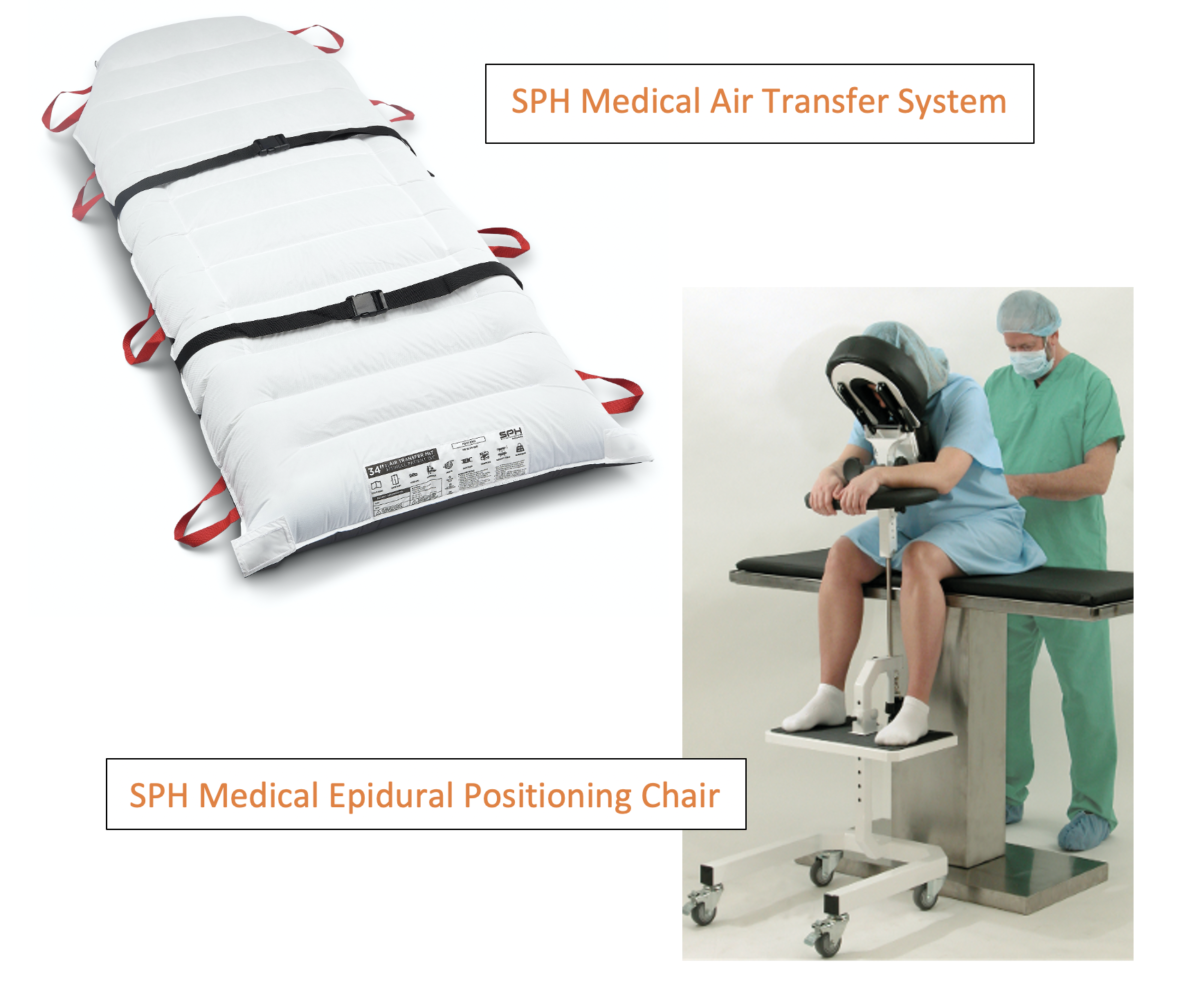
Are you looking for a way to keep your patients and hospital’s medical staff safe? Do you want to lower the risk of injuries while helping patients get better faster? The epidural positioning chair may be the answer. Known as the Epidural Chair or the Epidural positioning device (EPD), the EPD is being used in hospitals and surgical practices to enhance patient safety. The device provides secure and comfortable, stable support for patients undergoing epidurals, spinal blocks, or lumbar punctures.
Many departments use EPDs for safe patient handling and to enhance worker safety in clinics, hospitals, and pre-op areas. The imaging and surgery department uses EPDs for comfort, to hold patients in positions for various procedures to reduce the risk of injury to technicians.
Epidural Chair: What is it?
People often mistake it for a chair, but it is actually the bed or table on which the patient is seated. EPD supports the arms, head, chest, and feet while a patient is seated. The device is portable and stable, allowing it to be used at the bedside as you prepare patients for spinal and epidural blocks. Various clinical settings, inside and outside of hospitals, can benefit from EPD. Epidurals are given almost every hour in labor and delivery rooms, and spinal blocks are now being administered even more often as the number of total joint replacements increases.
Epidural Positioner: Ease of use and maintenance
The Epidural Positioning Chair provides a better solution for nurses, medical staff, and health care facilities. Many hospitals consider positioning patients as the standard of care that minimizes the risk of falls, sprains, and injuries. The EPD can be used for epidurals, spinal blocks, thoracentesis, and other pain management procedures.
With EDP, patients can receive spinal blocks or other epidural therapies in a more private, dignified way. This is also safer for caregivers. The armrests adjust in six positions, and the headrest can change 180 degrees. The device can easily fit operating rooms, birthing rooms, clinics, labor and delivery rooms, and imaging departments. Disposable covers make it easy to disinfect and clean the EPD’s face rest.
EPD: The Benefits
During, after, and before the COVID-19 epidemic, thoracentesis became routine. Epidural positioning devices make the process simpler and more predictable. According to an expert, thoracentesis usually involves the patient leaning forward while their arms rest on a bedside table. Patients who cannot sit will lie on their side for safety.
Ultrasound techs also need a safe working environment. Syncope caused by vasovagal responses during thoracentesis can be treated safely with the EPD. Studies show many hospitals and medical centers use the EPD for thoracentesis procedures. It is also very popular with technicians and patients alike. In studies of pregnant women who received epidurals, women found that positioning devices made them feel more comfortable.
Compared to the patient satisfaction before using the devices, patient satisfaction increased significantly. Other benefits include:
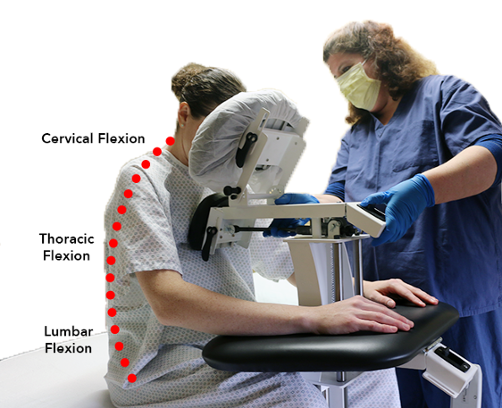
- Maintains correct thoracic, cervical, and lumbar flexion to maintain stable alignment.
- Provides a more private and less intrusive position for the patients
- Help to prevent injuries to medical and anesthesia staff.
- Wheeled for easy mobility
- Easily fits any patient
- Increases patient satisfaction
Eliminate Manual Handling with The Epidural Chair
Nurses and caregivers manually position patients for epidural procedures in preoperative settings, operating rooms, and the hospital at large. During most procedures, caregivers must hold a stool, table, and patient steadily with their entire bodies. This prevents the patient from moving, resulting in an injury. When the medical assistant is assisting the patient in holding a flexed spinal position, they are potentially putting themselves in a risky position.
Handling patients manually puts medical staff at risk for musculoskeletal injuries. As part of perioperative procedures, staff members position patients as needed for spinal and epidural blocks, respectively, in Pre-Op, OR, and other rooms as required. Most patients sit at their bedsides and place their feet on a portable stool on wheels by the bedside. To create the “mad cat” flexed spine position, the nurse brings a non-locking bedside table to the patient and places pillows as needed on it. Sometimes, the patient is simply leaning forward while their arms are wrapped around a stack of pillows. By holding the foot stool in place, the nurse keeps the patient’s upper body stationary while holding the foot stool in place with the knees or thighs. The nurse or nurse assistant must often support some of the patient’s body weight during needle insertion.
Further complicating the situation, patients are often in pain, nervous, and unpredictable, putting the staff at risk. Several hospitals have concluded that prolonged holds and counterpressure tasks are high risk. They have redesigned epidural and spinal block placement processes to eliminate manual patient handling based on their predictable daily routine.
Besides reducing risk to the medical staff and caregivers, the Epidural Positioning Device creates a comfortable and safe needle placement position, ensuring increased patient comfort. Experts have shown that “normal” patients suffer injuries when they are handled manually. The constant turning, lifting, pulling, pushing, and transferring has the cumulative effect of causing small tears in the joints and discs, leading to injury.
Safeguarding the medical staff
Strain, back injuries, and other musculoskeletal disorders (MSDs) are a severe concern for healthcare workers. The Association of Perioperative Registered Nurses (AORN) estimates that around 50 percent of all non-life-threatening injuries sustained by nurses are MSDs, with approximately 25 percent of these injuries involving the back.
The EPD typically addresses these concerns in preoperative rooms, which are prone to injuries. Studies show many prestigious hospitals use the device, including Mayo Clinic, VA Medical Center, Duke University Hospital, and Kaiser Hospitals. This device is an invaluable asset to the imaging team, perioperative, and Labor and Delivery (L&D), a win-win for everyone.
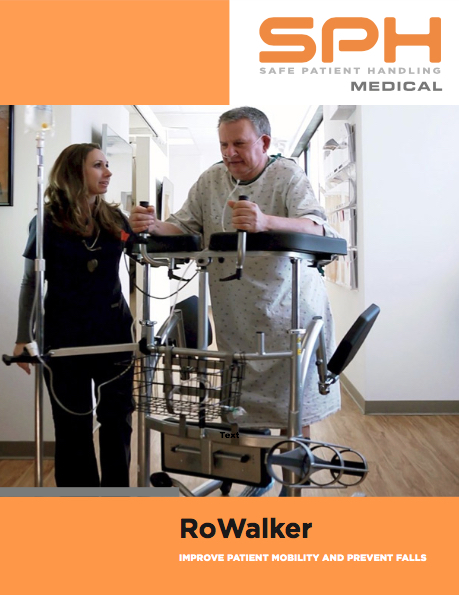
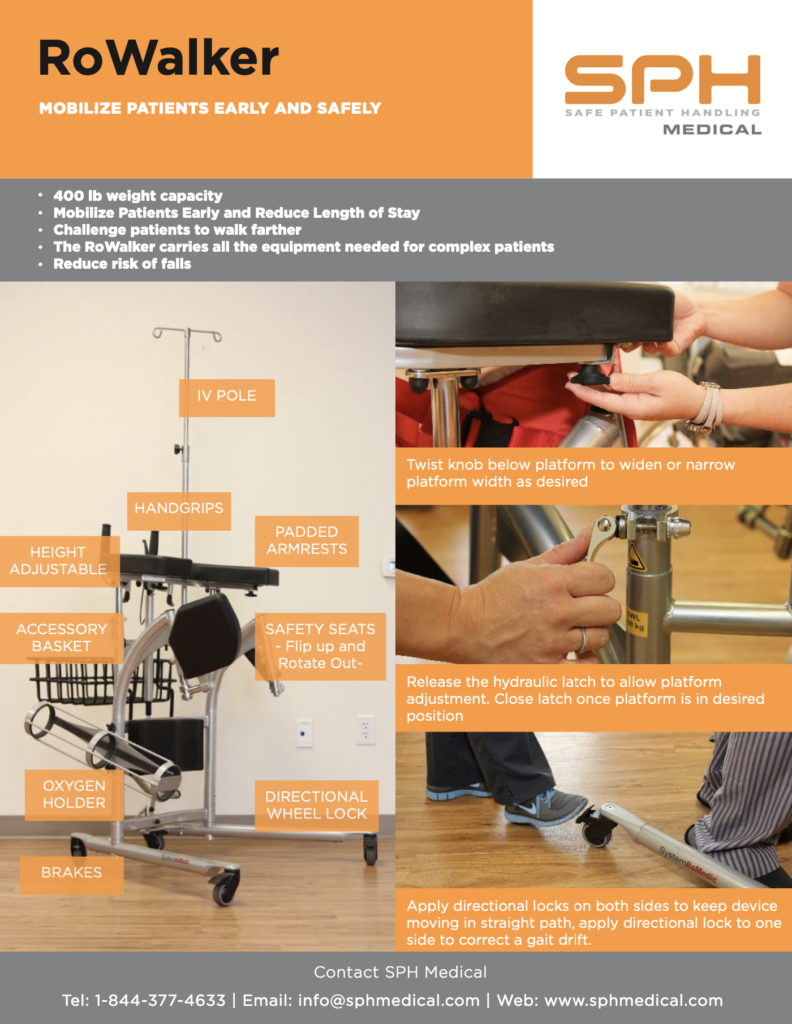
With the EPD, you can immediately and effectively increase patient and staff safety. If you would like more information or to request a quote, contact SPH Medical. The primary focus of SPH Medical is the safety of nurses and caregivers. The national organization offers a wide selection of safe patient handling products to healthcare facilities and hospitals nationwide, such as patient lifting solutions, air assisted transfer and positioning systems, patient slings, Nitrile Exam Gloves, N95 masks, and disinfection products.