An epidural is a frequent procedure used to offer pain relief or numbness during labor and childbirth and some surgeries and chronic pain. An epidural pain relief is a technique that involves injecting a medicine into the spine’s epidural space, either an anesthetic or a steroid. This technique is used to offer pain relief or a total loss of feeling in a specific area of your body, such as your legs or abdomen. It aids in blocking pain signals from the spine to the brain. The anesthetic blocks pain signals by numbing the spinal nerves. It relieves discomfort for women in labor or having a cesarean section. This anesthetic is particularly effective at blocking discomfort from labor contractions and during delivery. You can normally move and control pushing of the baby when you have an epidural.
The Epidural Positioning Device
A distinguished anesthesiologist created the first epidural positioning device about two decades ago to improve patient and staff safety. The EPD has now become the gold standard of positioning devices. The Surgery Department and the Labor and Delivery Unit benefit the most from this development.
When it comes to positioning patients safely and decreasing the risk of injury to caregivers and medical personnel, the device helps keep patients safe while also reducing the risk of injury to caregivers and medical staff. The EPD is most commonly used to position a patient for an epidural placement but is also used in other areas of the hospital to position patients. The EPD has numerous advantages for both nursing staff and caregivers.
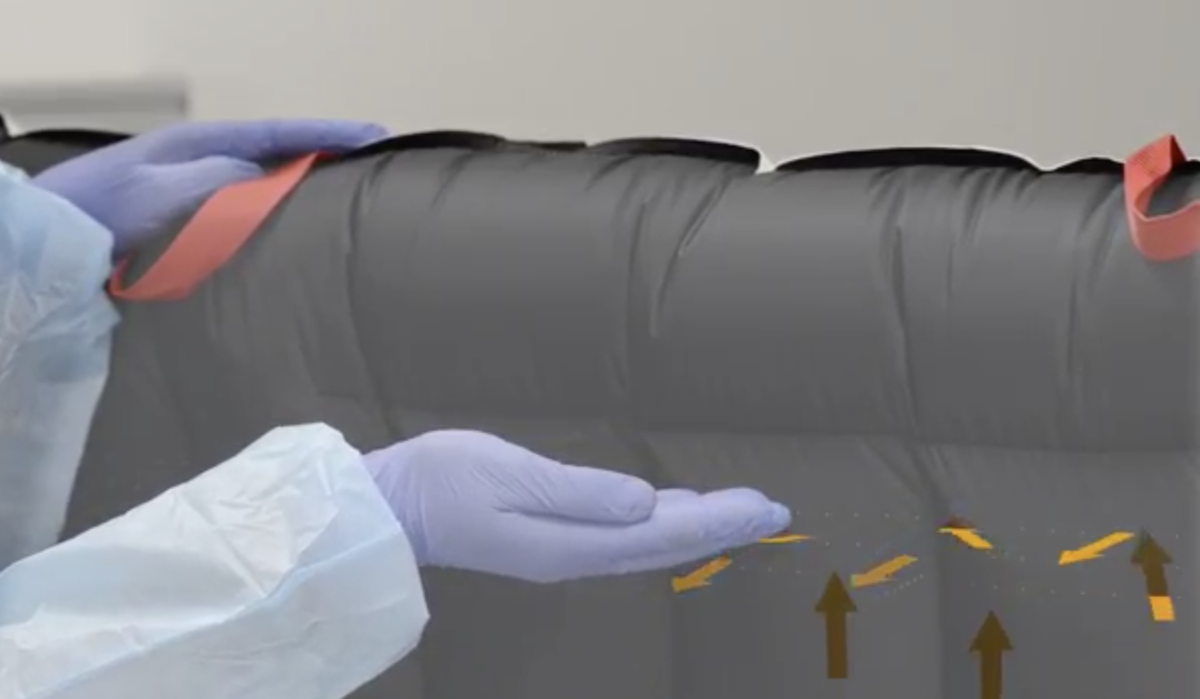
An epidural chair has a stable foundation. It quickly locks into place and has several adjustable features to ensure that each patient is in the best possible posture for the treatment. The following adjustable features:
- Height adjustability
- Tilting Paded Face Rest Cushion
- Foot Plate
- Depth Adjustable Chest Cushion
- Arm Rests
- Locking Wheels
Why Is Proper Positioning Important for Epidural Pain Relief
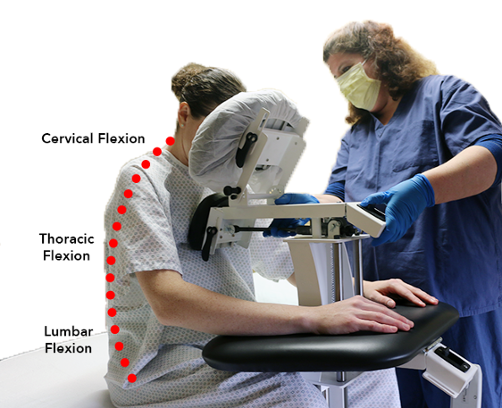
The Epidural Chair improves safety by appropriately positioning and supporting a patient for a successful procedure, the first and most visible advantage.
Complication risk is reduced. There is a considerable risk of complications due to the unique and strenuous nature of patient posture during spinal blocks and epidural treatments. With this device, caregivers don’t have to rely on their body positioning to keep the patient secure.
Anesthesiologists have also used the technology for various types of spinal blocks as a result of its success in delivery aid, providing epidural pain relief during various procedures.
What is Epidural Pain Relief and What Is the Risk to The Patient?
In the past, the nurse or medical assistant was responsible for manually positioning the patient, which increased the risk of injury or musculoskeletal disorders (MSDs). Assisting with epidural procedures is one of the known high-risk tasks for nurses. Modifying the task or implementing engineering controls to eliminate the risk is the greatest strategy to lessen the chance of injury. Your team will benefit from the positioning devices engineering control and risk reduction.
Patients benefit from an epidural positioning device because it provides a stable base. When the patient is positioned correctly, the caregiver can rely on the device rather than their body weight to keep the patient in the best posture for the treatment. These advantages significantly minimize the risk of problems during a spinal block and epidurals.
Patient Positioning Challenges
- During epidural and spinal block placements, clinicians in the Labor and Delivery Unit, Surgery Department, and pain clinics face various demanding scenarios.
- Holding a patient in place poses a risk to the staff’s safety.
- Pillows stacked on non-locking tables endanger patients’ safety.
- Patients on medication may find it challenging to maintain the correct position.
- Keeping a stool in place while supporting a patient is a difficult task.
- Patients may have an unanticipated reaction and try to move.
- Patients may feel dizzy or queasy, causing them to move around.
With this Epidural assisting device, the patient is in a safe, secure, and comfortable position. It is the responsibility of hospitals and medical facilities to ensure the safety of their nurses and support staff. Providing the necessary equipment is part of the plan to keep employees injury-free. While assisting with traditional positioning methods connected with epidurals and similar procedures like spinal blocks in the OR and Thoracentesis in the imaging department, positioning devices reduce over exertion, body strain and risk of injury to nurses. It’s critical to keep nurses and hospital workers in good health to function at their best.