When most people think about the effectiveness of modern healthcare, they think about innovative robotic surgeries or new medications. While these advancements certainly are relevant, they are not the only advancements that improve patient outcomes and increase staff safety during epidurals or procedures. One of the most recent innovations is an epidural positioning device.
Known more commonly as an EPD, this device is designed to provide better support for patients during the administration of an epidural or spinal block. An epidural positioning chair is most likely to be employed by an anesthesiologist and nursing staff to provide optimal spinal, lumbar, or cervical flexion. The patients will also see direct benefits.
The need for proper positioning relates to how an epidural is administered. The epidural injection occurs in the space between the spinal column and outer membrane of the spinal cord also known, as the epidural space, in the mid to lower back. The flexed spine position opens up this space. Epidurals are perhaps best known as a tool for pain control or analgesia during labor and delivery. Spinal blocks are similar procedures. However, a spinal block is a single shot in the dural sac. The relief is fast and effective. That is why a spinal block is common in general surgery.
Staff Safety During Epidurals wit the EPD
Despite the large volume of these procedures, the process of positioning patients today remains a manual and risky process for nursing staff during epidurals. Traditionally, patients must be moved in either a side lying position or leaning over a woefully unstable bedside table with pillow to enable spinal flexion and to provide access to the spine. Often, nursing staff must manually position patients and hold them in place. This requires a lot of manual static holding, counter-pressure, and other manual pushing and pulling, which puts the support staff at risk of a musculoskeletal injury. Over time, this can lead to muscle or joint disorders that cause long-term impairment or pain. The risk to staff is often overlooked on the Labor and Delivery unit where nursing injuries are increasingly problematic for both employees and costly for hospitals.
pushing and pulling, which puts the support staff at risk of a musculoskeletal injury. Over time, this can lead to muscle or joint disorders that cause long-term impairment or pain. The risk to staff is often overlooked on the Labor and Delivery unit where nursing injuries are increasingly problematic for both employees and costly for hospitals.
Moreover, this process can be quite uncomfortable for patients. The idea of getting a shot in the spine can already be unnerving for some patients. The manual process of being held in place can increase any associated anxiety. Plus, since the process is done manually, there is some risk of movement or error. Patients often have higher comfort levels when they feel stable, properly supported, and secure.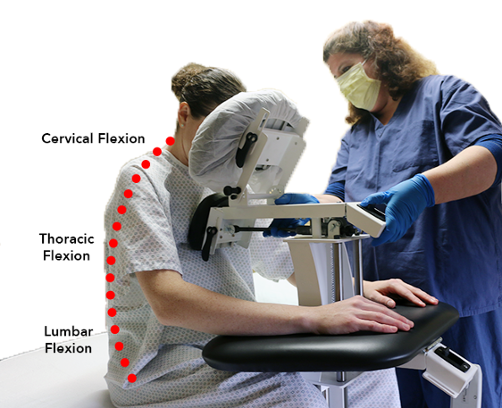
In this manner, the EPD solves problems from both ends. With an epidural positioning device, patients can be properly positioned without manual patient handling that puts nurses at risk of injury. Instead, patients are comfortably positioned with adjustable arm rests, a face rest and a foot plate so they can comfortably remain still while the anesthesiologist has direct access to the spine. Patients are far more comfortable, and the risk of injury to staff is dramatically reduced.
Epidural Positioning Chair
The applications for the epidural positioner are vast. They can easily be incorporated into the labor and delivery unit for expectant moms. The EPD has also gained a great deal of popularity in surgical departments across the globe. These positioners can be used to help patients prepare for common joint replacement surgeries where spinal blocks are a normal part of the standard of care.
Now, the positioners are even being purchased for use in imaging departments. There is a growing consensus that the use of a positioner can be useful during a thoracentesis. This unique procedure requires the doctor to insert a needle through the chest wall. The needle is then directed to the space between the lung and the chest wall. In some conditions, fluid can accumulate in this area. This is known as pleural effusion, and it can make it difficult to breathe. A thoracentesis, therefore, will ease the pressure on the lungs while also making it easier to diagnose the cause of the fluid buildup.
The EPD Providing Staff Safety
Given the precise positioning needed to complete a delicate procedure like a thoracentesis, the use of a positioner has obvious benefits. It is easier to get the patient into the correct position, and the positioner ensures that the patient does not shift or move during the procedure. When the process involves the use of needles in a sensitive area, secure precision is preferable.
In the end, medical advancements come in all shapes and sizes. While a positioner may not seem as dramatic as some breakthroughs, the benefits of the Epidural Positioning Chair cannot be overstated. To improve staff safety during epidurals and to increase patient comfort, the advantages make a clear argument for increased usage and broader implementation. New applications are continuing to be discovered, and it is clear that the EPD deserves a place in hospitals worldwide.