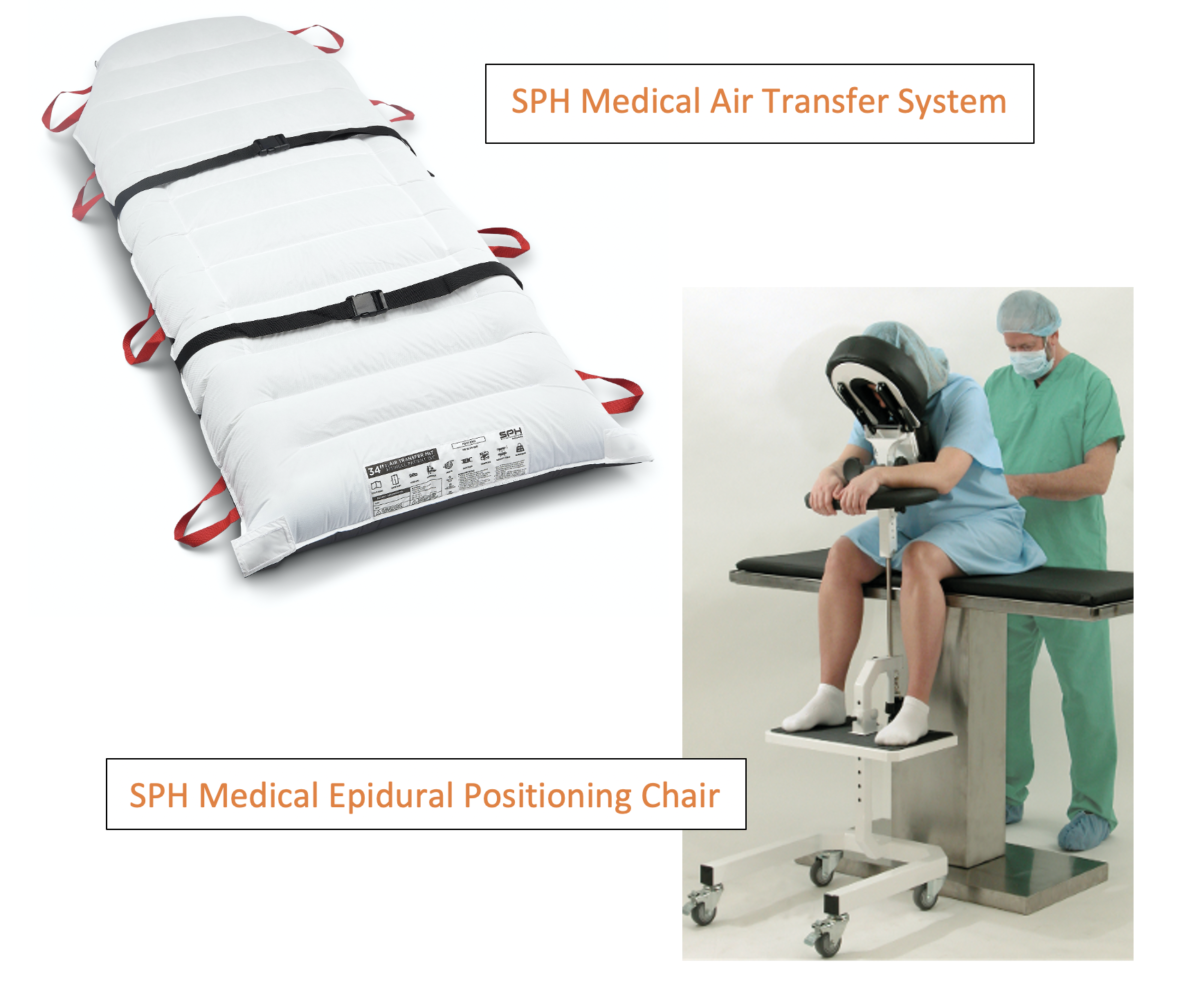
Across the globe, the SPH Medical’s Air Transfer System (ATS) keeps patients and caregivers safe. We provide a full range of widths and lengths to suit your hospital’s safety program with the highest quality control, backed by a manufacturer’s warranty and safe patient handling education. Performing patient transfers, repositioning up in bed, turning from one position to another is a daily task for nurses. Even though it is routine and done frequently, moving patients can be a challenging task that can cause injuries to staff and patients. The single patient use air mattress is a prominent transfer device. Research has shown that air-assist technology has many benefits. With a number of air transfer systems available, it can be difficult to choose the right one for you. To emphasize the importance of safe patient handling, we have compiled a top ten questions from direct customer questions and feedback.
Q: 1. How do air-assisted transfer systems work?
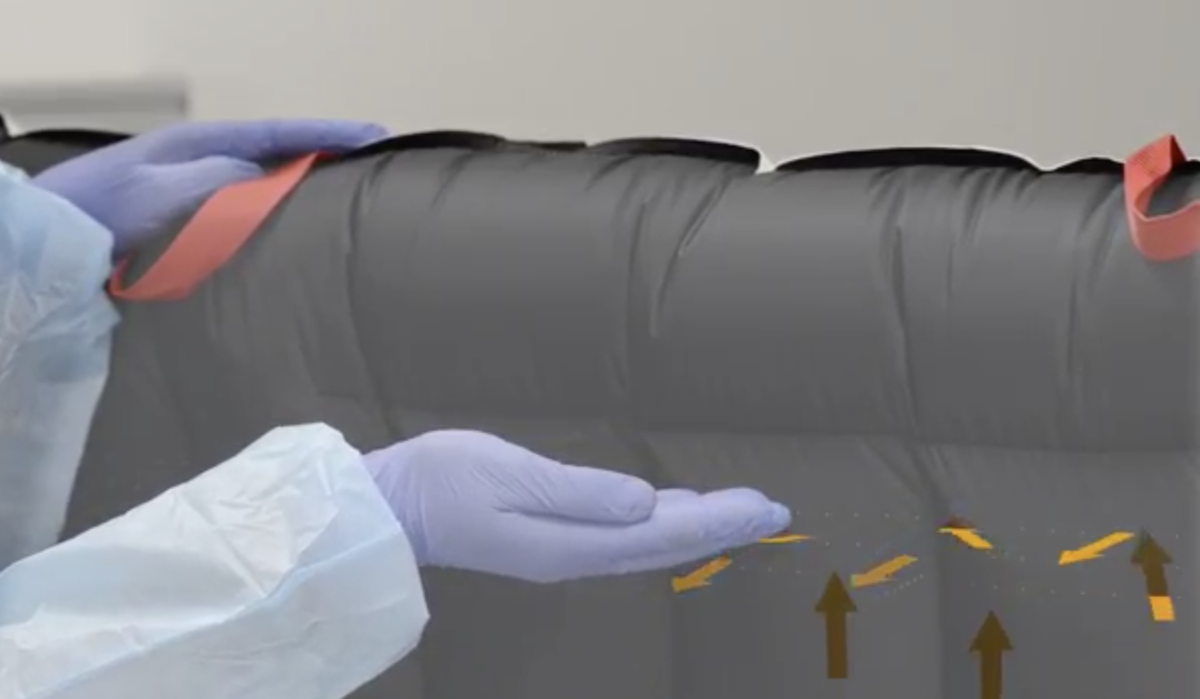
A: The Air Transfer Mattresses have many small air hole perforations that allow air to escape when the motor or air supply inflates the mattress. As a result of the air passing through these holes, the mattress will have less friction against the bed surface. With low friction, it is easy to transfer the patient. When two surfaces are separated by air, they move freely like a tabletop air hockey game or hovercraft.
Q: 2. What are the main components of the Air Transfer System?
A: The main components include the mattress, hose assembly, air supply or blower unit, ergonomic handles, and patient safety straps.
Q: 3. Which is more common the Single Patient Use or Launderable version?
A: A patient’s or medical facility’s laundry system and capital budget planning may determine whether the air transfer systems deployed are single patient use or Launderable. Hospitals that tend so send their laundry out to third part laundry providers often find that their hospital owned goods get lost by their laundry providers!
Many hospitals have lost hundreds of thousands of dollars worth of slings and transfer mattresses. For this reason the Single Patient Use Air Transfer Mattress has gained significant popularity. Avoiding that horrible laundry system and being able to keep track of inventory on the shelf allows you to track actual usage which directly correlates to risk avoidance and reduced injury costs!
Capital budgets can be difficult to navigate for those in charge of Safe Patient Handling programs as they compete with other hospital priorities to purchase new life saving equipment or revenue generating solutions needed by various departments. Although the investment in patient lifts, slings, mobility solutions, and Air Transfer Systems is an essential need it often falls behind these other priorities. If there is a concerted effort by a team of leaders from all departments including Nursing, Physical Therapy, Surgery, and Imaging these essential purchases can be prioritized and eventually made after lengthy budget planning.
The Single Patient Use Transfer Mattress is a much easier item to deploy for this reason. It is a supply item. Each department can place their order weekly or monthly and get the supplies they need and this typically avoids the entire capital budgeting nightmare. With SPH Medical Air Transfer Mat, adopting this gold standard technology has never been more affordable.
With SPH Medical, you will find a complete range of Air Transfer solutions, including single patient use and durable options. They are expert at Safe Patient Handling and understand the unique injury risks and needs of each and every type of patient care environment. Their experience includes implementing a complete range of solutions in Labor and Delivery, ICU, Med Surgery, Imaging, General Surgery, Rehab, and many other departments.
Q: 4. How does the system reduce the risk of injuries to nurses?
A: Hospital staff who perform frequent repositioning tasks or lateral patient transfers are at risk of suffering a back injury. These high frequency tasks are predictable and the old fashion way of manually boosting, turning or transferring patients is a well known cause of career ending back injuries. Although lower severity back injuries along with strains and sprains are common and often do not receive much attention, these injuries cause facilities significant losses in productivity and money. The Single Patient Use Air Transfer Mattress improves nursing efficiency and improves patient care by reducing the need for 3-4 nurses to perform a task. For manual handling or alternative non-air friction reducing devices, it takes at least three hospital employees to transfer a patient, but with the Air Transfer System it only take two. This increased efficiency means that they nurses can perform other tasks or attend to their other patients rather than being constantly called to assist.
Q: 5. Is the single Patient Use version breathable (Can it be left under patients)
A: SPH Medical has conducted thorough pressure mapping, and breathability testing on its Single Patient Use Air Transfer Mat to ensure that it is safe for patients as well as caregivers. Based on pressure mapping and moisture vapor transmission testing, there is minimal impact to the support surface and patient when lying on the Single Patient Use Air Transfer Mat, making it safe to leave it under patients all day.
Having housekeeping staff make the unoccupied bed with the Air Transfer Mat means that nurses have the ability to boost, turn, and transfer whenever needed. This increase in availability and accessibility equals improved safety for nursing staff.
Q: 6. Does the motor or Air Supply go with the patient during transport (on the bed or gurney)?
A. Yes. The SPH Medical Air Supply has convenient hooks on the back that allow it to hang on the foot of the bed or the stretcher. In some cases the transport staff moving a patient will put the air supply underneath the stretcher if there is space. Several transport carts and stands are available to hold the Air Supply and Single Patient Use Transfer Mats. Some hospitals prefer to leave the Air Supply in each department so you just use the Air Supply at the destination end to transfer or move the patient. In this scenario where the entire hospital has Air Supplies you never need to bring it with you.
Q: 7. Can the Air Transfer System be left under patients during X-Ray or CT Scan?
A: Yes. The majority of air transfer mattresses are safe and radiolucent and offer a safe environment for imaging procedures and x-rays. If you are requesting information on a product, confirm with the company.
Q: 8. What is the typical cost for a Single Patient Use Air Transfer mattresses?
A: Price ranges typically range from $75 to $100 each, depending on contract relationships and volume purchases, without including Air Supply and Transport Stands.
Q: 9. What is the Return on Investment realized when implementing a hospital-wide Air Transfer and Positioning solution?
A: Air Transfer and positioning solutions can help reduce injuries, costs, and resources. Hospitals can save hundreds of thousands of dollars on direct injuries with the implementation of Air Transfer and positioning solutions. But indirect injuries have been estimated, but indirect injuries cost three to ten times as much.
A national survey of 1,000 hospitals shows that patient handling injuries account for 25 percent of workers’ compensation claims. Patient handling injuries are the most expensive type of hospital workers’ injury. Along with direct expenses, hospitals have indirect costs that are hard to measure but have a tangible impact on finances and resources. These include overtime, training, productivity, morale, employee turnover, and incident investigation time.
Q: 10. Are air-assisted devices safe for handling patients?
A: An Air Transfer System is one of the safest transfer and repositioning solutions available today. This proven technology has now been in use for more than 30 years and has been implemented on virtually all hospital units where repositioning, turning, and lateral transfers occur. There are other injury prevention solutions that are currently used in hospitals to lift move and transfer patients but nurses and technical staff have reported that the Single Patient Use Air Transfer Mattress is the most convenient and user friendly Safe Patient Handling solution. Today the SPH Medical Air Transfer System is considered the gold standard of patient transfer systems.
In addition to being safe for caregivers, the single patient use Air Transfer Mattress has become a key component of the hospital infection prevention plan. Even prior to COVID-19 the hospitals have been focused on the reduction of HAI’s or Hospital Acquired infections. The Single Patient use version of the Air Transfer Mattress stays with the patient during their entire length of stay and when soiled, or the patient is discharged, the item is thrown away. No laundering or messy spray and wiping disinfection is required.
It is also important that the mattress inflates at the perimeter before inflating at the center. As a result, the patient rests in a cradle, which reduces the chances of tipping over.