The SPH Medical Epidural Positioning Chair is improving patient satisfaction across the country. Procedural anxiety is a universal challenge in healthcare. For patients undergoing spinal blocks, epidurals, or thoracentesis, the fear of pain is often compounded by physical discomfort. It’s not easy to maintain a rigid, awkward position for minutes at a time. Traditional positioning methods often involving pillows, bedside tables, or physical support from a nurse, are frequently unstable and uncomfortable. Given this, there is increased patient stress and potential movement during critical moments. This instability creates a cycle of anxiety and physical strain that can negatively impact the entire procedure.
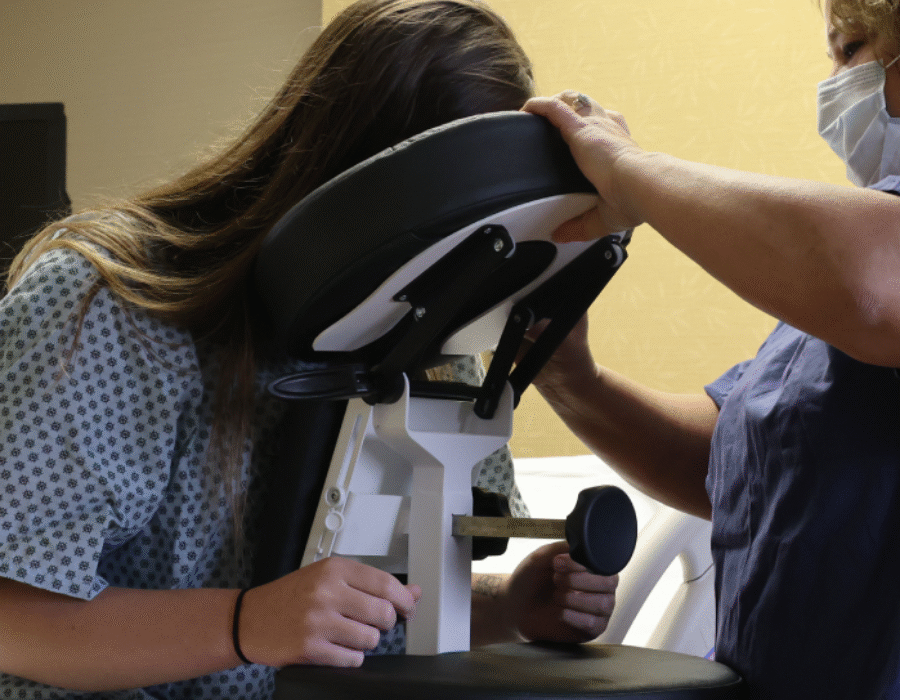
The Epidural Positioning Device (EPD), also known as the Epidural Positioning Chair, revolutionizes the patient experience by providing ergonomic, stable, and customizable support. It transforms a high-stress procedure into a controlled, comfortable environment, directly improving patient satisfaction scores and enhancing clinical outcomes.
This article will explore how the EPD addresses the specific comfort needs of patients across various procedures, minimizes anxiety through unparalleled stability, and serves as a vital tool for improving the overall quality of care and the patient experience.
The Anxiety of Instability: Why Traditional Positioning Fails Patients
Patient comfort is not a luxury; it is a clinical necessity for procedural success. When patients are uncomfortable or feel unstable, their anxiety levels rise, which can heighten pain perception and increase the likelihood of sudden movements. Traditional methods of positioning often fail to provide the consistent support needed to ensure a calm and stable environment.
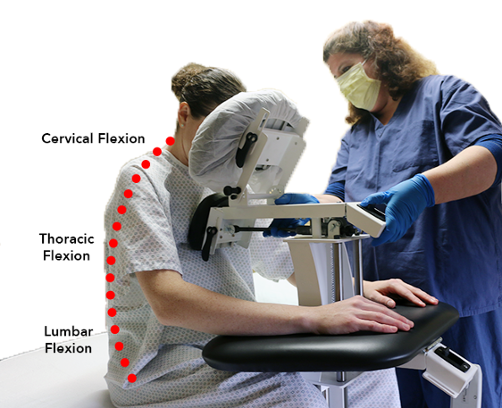
The physical and psychological strain on patients asked to “curl forward” or “stay still” on the edge of a bed without adequate support is immense. For pregnant, elderly, or bariatric patients, maintaining the “tripod” position independently is physically exhausting and often impossible. This struggle to remain still creates deep-seated psychological anxiety. The fear of moving and causing injury or prolonging the procedure is a significant stressor that can impede a successful outcome. Even when a nurse provides manual support, this well-intentioned assistance cannot replicate the rigid, unwavering stability of a mechanical device, often leaving patients feeling insecure and vulnerable.

Ergonomic Engineering: Designed for Diverse Patient Needs
The Epidural Positioning Chair is meticulously engineered to accommodate the unique anthropometrics of a diverse patient population. As such, the EPD ensures dignity and comfort for every individual. It was designed from the ground up to solve the core challenges of procedural positioning by providing a fully customizable support system.
The EPD’s adjustable features are specifically designed to maximize patient comfort and promote the ideal posture:
- Adjustable Face Support: This prevents severe neck strain and allows for relaxed breathing. The Face Rest Cushion or holding the head in an unnatural position.
- Ergonomic Arm Rests: These supports remove tension from the shoulders and upper back, allowing the patient to relax fully instead of tensing their muscles to maintain balance.
- Integrated Foot Rest: The adjustable footrest provides grounded stability, which is essential for patients of all statures. It prevents the feeling of dangling and adds another point of secure contact, reducing dizziness and lightheadedness.
Furthermore, the EPD’s high weight capacity and wide, stable footprint provide dignified and secure support for bariatric patients, a population often underserved by standard medical equipment. The device ensures that every patient, regardless of their size or physical condition, can be positioned safely and comfortably.
Stability Equals Serenity: Reducing Anxiety Through Unwavering Security
When a patient feels physically secure, their psychological anxiety diminishes, leading to a smoother, safer, and more efficient procedure. The EPD provides a level of stability that manual holding can never achieve, creating a profound sense of serenity for the patient.
The secure chest support and solid overall structure of the Epidural Positioning Chair provide a sense of being held or “hugged,” which has a powerful calming effect on patients. This feeling of being safely enveloped by the device helps to reduce heart rate and blood pressure associated with anxiety.
Most importantly, the device virtually eliminates involuntary movements. A patient who is mechanically stabilized is far less likely to flinch, startle, or shift their weight during a critical moment. This dramatic motion reduction minimizes the risk of needle readjustment and multiple puncture attempts. Of course multiple attempts are significant sources of patient pain and dissatisfaction. The unparalleled stability provided by the EPD is directly linked to faster procedure times, fewer complications, and a dramatic improvement in patient satisfaction and HCAHPS scores.
Versatility in Comfort: One Epidural Chair, Multiple Procedures
The profound comfort benefits of the Epidural Positioning Chair extend far beyond obstetrics to a wide range of critical bedside procedures, making it one of the most versatile tools in any facility.
- Epidurals and Spinal Blocks: For neuraxial anesthesia, achieving optimal spinal flexion is critical for success. The EPD encourages the ideal curvature of the spine effortlessly and comfortably. By supporting the patient’s weight, it allows them to relax into the ideal position. The chest cushion also helps promote the flexed spine position for the anesthesiologist. This makes the procedure faster, less painful, and significantly more successful on the first attempt.
- Thoracentesis: This procedure often requires patients to sit still in a forward-leaning position for an extended period. The EPD is the perfect solution, allowing patients to rest their entire upper body weight comfortably on the device. This support reduces fatigue and minimizes the risk of a vasovagal response (fainting), which is a common complication when patients become tired or anxious.
The Epidural Positioning Chair is more than a positioning tool; it is a patient experience solution. By replacing instability and discomfort with ergonomic security and stability, it directly addresses the root causes of procedural anxiety. It provides a consistent, reproducible, and comfortable environment that empowers patients to remain calm and still, contributing to better clinical outcomes.
Investing in the EPD demonstrates an unequivocal commitment to a higher standard of patient care. It ensures that every patient, regardless of their size, age, or mobility level, feels safe, supported, and respected during their most vulnerable moments. It is an essential technology for any facility dedicated to maximizing patient satisfaction and clinical excellence.
Elevate your standard of care and improve your patient satisfaction scores. Contact SPH Medical today to discover how the Epidural Positioning Device can transform the patient experience in your facility.