The Epidural Positioning Chair Improves Safety
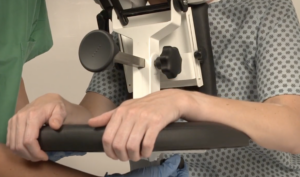
The Epidural Positioning Device (EPD) is used to help patients get an epidural injection. The design is intended to improve the safety of these procedures by reducing the risk of accidental dural puncture and increasing comfort for patients. It does this through its four-point support system, which stabilizes a patient in a seated position during their procedure with padded armrests, face support, chest cushion, and foot rests on either side of them. The epidural pain relief procedure is a common way to provide pain relief during labor.
The epidural chair is used in Labor and Delivery unit and surgical departments because it’s effective at improving safety by improving patient stability and comfort. One of the most common solutions for pain and discomfort in pregnant mothers is epidural analgesia. This involves administering drugs through an epidural needle into the space around the spinal cord. This provides pain relief for the mother during labor. The medications used in epidural analgesia can also help speed up labor. In general Epidural Analgesia is very safe. There are some minor risks of side effects and complications for patients including low blood pressure, which can lead to a feeling of light headedness, and in some cases a temporary loss of bladder control
.1)Use of Epidural Device
The epidural chair is a simple yet effective device that helps improve the safety and comfort of patients receiving an epidural injection. The chair is portable on wheels enabling it to be moved easily into any area of the facility. The EPD is height adjustable adapting to each unique patient to support them in a comfortable position. This secure platform ensures that the patient stays safe and comfortable during the procedure. The epidural chair is available in many hospitals and clinics, and it can help make the process more comfortable for the patient. If you are scheduled for an epidural injection, be sure to ask if the hospital or clinic has an epidural chair available. This can help ensure that you have a safe and comfortable experience. The epidural pain relief procedure may also be performed in the surgery departments or in pain management clinics to relieve chronic pain.
2) Importance of Proper Epidural Positioning
Proper epidural positioning is important because it can help reduce the risk of accidental dural puncture and ensures a more accurate epidural placement. An accidental dural puncture is a severe complication when the needle used to give the epidural injection goes too deep and enters the space between the vertebrae and the spinal cord, called the dura mater. Spinal fluid can leak out when this happens and cause minor headaches to severe complications, including paralysis. Proper positioning and a comfortably stabilized patient can help ensure that the anesthesiologist is able to direct the needle into the correct position and doesn’t go too deep.
3) How does the EPD benefit the patient during the Epidural procedure?
The EPD is designed to properly position a patient in the ideal “mad cat” position that opens up the vertebral spaces for epidural placement. Patients are often nervous and scared when thinking about getting an epidural so the EPD really offers a comfortable and stable platform for the patient to lean on and hold. This makes it a valuable tool for hospitals and clinics to improve patient safety during epidural injections and spinal blocks. The Epidural Positioning Chair is used in Labor and Delivery departments and surgical areas because it’s effective at improving safety while still being comfortable.
4) Why Are Nurses at Risk of Injury During This Procedure, And How Does the Epidural Positioning Benefit Them Specifically?
Nurses are at risk of injury during this procedure because they are typically handling patients manually and having to position the patient in a side lying position or manually positioning a patient at the edge of the bed while supporting the patient as they lean on pillows stacked on an unstable bedside table. The nurse would also be likely holding the stool in place to support the patients feet with his/her own foot. What happens when a patient suddenly moves or passes out and falls to the floor? The nurse often has to catch the falling patient or apply counterpressure to help the patient maintain the correct body position. This manual handling process is outdated and unsafe. The EPD solves all of these issues.
Conclusion
Using the Epidural Positioning Device to improve safety and comfort for patients getting an epidural injection or spinal block is vital in preventing injury to nurses and patients. The epidural device helps reduce the risk of severe complications during these procedures by providing a comfortable and safe way to position patients. Using the device to improve safety and comfort for patients getting an epidural injection or spinal block is vital in preventing injury to nurses and patients. The device helps to reduce the risk of serious complications during these procedures by providing a comfortable and safe way to position patients. Proper positioning is important because it can help reduce the risk of complications and to ensure optimal patient outcomes. An epidural positioning device is considered an essential piece of equipment in Labor and Delivery Unit and surgery departments today.