Over the past decade, an air transfer system has become increasingly popular in healthcare settings as an effective solution for reducing nursing injuries. These innovative systems have been credited with significantly lowering the number of nurse-related injuries and workers’ compensation claims, while increasing patient safety and comfort. By utilizing advanced technologies and ergonomic design, air transfer systems provide a safe, easy, and efficient means of patient transfer that surpasses traditional methods. In this article, we will take a closer look at the many benefits of air transfer systems and why they have been so successful in revolutionizing patient care.
Safe Patient Transfer
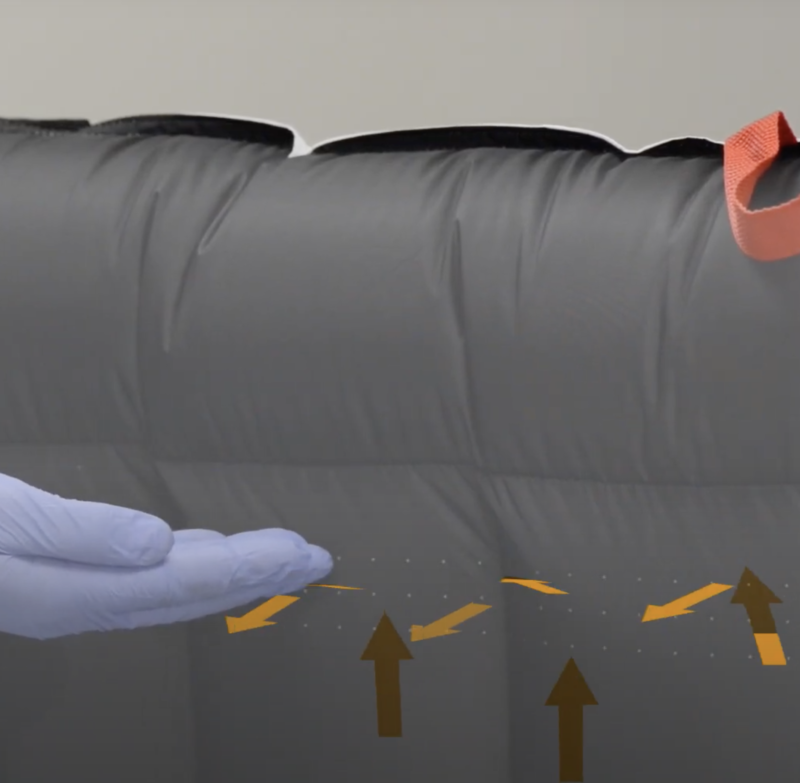
An air transfer system provide a safe solution for patient transfer, minimizing the risk of injury to both patients and healthcare workers. Traditional methods of patient transfer often involve physical lifting and maneuvering, which can result in back injuries, muscle strains, and other debilitating conditions. By contrast, air transfer systems utilize a cushion of air to lift and move patients smoothly and effortlessly, reducing the likelihood of injury to both the patient and the caregiver. These systems are also designed with safety features such as locking brakes and adjustable height settings, ensuring optimal positioning and stability during transfer.
Easy to Use and Efficient
Air transfer systems are incredibly easy to use, requiring minimal physical effort on the part of the caregiver. With just the push of a button, patients can be effortlessly moved from one location to another, minimizing discomfort and maximizing efficiency. This streamlined approach to patient transfer not only saves time but also reduces the risk of errors or accidents during the transfer process. Additionally, air transfer systems are designed to fit a wide range of patients and care settings, making them a versatile tool for any healthcare environment.
Improved Patient Comfort
Another key benefit of air transfer systems is the improved comfort they provide for patients during transfer. Unlike traditional methods that can be uncomfortable and even painful, air transfer systems offer a gentle, smooth transfer that minimizes jarring movements and reduces the risk of pressure sores or other injuries. Patients can remain in a comfortable seated or lying position throughout the transfer, ensuring their safety and well-being. With air transfer systems, patients can experience a higher level of comfort and care, improving their overall satisfaction with the healthcare experience.
Cost Effective Solution
Not only are air transfer systems highly effective in preventing nursing injuries, but they also represent a cost-effective solution for healthcare providers. The direct cost of nursing injuries can be substantial, with workers’ compensation claims, lost productivity, and medical expenses all contributing to the financial burden. However, by employing air transfer systems, healthcare organizations can significantly reduce these costs by minimizing the risk of injury and improving patient outcomes. Perhaps even more importantly, air transfer systems can have a significant impact on the indirect costs of nursing injuries, which are estimated at 5-10 times the direct cost. By investing in air transfer systems, healthcare providers can save money while providing safer, more efficient care to their patients.
SPH Medical’s Disposable Air Transfer System
SPH Medical’s single patient use air transfer mats provide a cost-effective and convenient solution for patient transfer while minimizing the risk of cross-contamination between patients. These disposable mats are compatible with all major blowers or pumps, and can be quickly and easily be deployed as a supply item, and disposed of when no longer needed, reducing the need for time-consuming cleaning and disinfection procedures. By using disposable air transfer mats, healthcare providers can save money on cleaning supplies and labor costs, while also reducing the risk of infection transmission between patients. Additionally, SPH Medical’s air transfer mats are designed to be both durable and comfortable for patients, ensuring a smooth transfer experience that promotes safety and well-being.
Conclusion:
In conclusion, air transfer mats are a highly effective solution for improving patient safety and reducing the risk of nursing injuries. SPH Medical’s single patient use air transfer mats offer a range of benefits that can save healthcare providers time and money while improving patient outcomes. These disposable mats are cost-effective, compatible with all major blowers or pumps, and can significantly reduce the risk of cross-contamination between patients. By working with SPH Medical to switch to single patient use air transfer mats, hospitals can realize significant cost savings while providing safer, more efficient care to their patients. With these innovative products, healthcare providers can improve patient outcomes, minimize the risk of injury, and promote a culture of safety in their organizations. Contact SPH Medical today to learn more about how their air transfer mats can benefit your healthcare organization.