In the ever-evolving landscape of surgical procedures, SPH Medical’s Epidural Positioning Device (EPD) stands as a beacon of innovation and safety. The EPD is an advanced tool designed to assist in the precise positioning of patients during spinal blocks a procedure gaining popularity in joint replacement surgeries due to its proven benefits. Studies have shown an increase in the use of spinal blocks, leading to improved patient outcomes, particularly in terms of pain management and recovery time.
A Deeper Dive with the Epidural Positioning Device: Why Surgeons are Opting for Spinal Blocks in Joint Replacement Surgeries
Recent trends in orthopedic surgery reveal a marked shift towards the use of spinal blocks, particularly for joint replacement procedures. This shift is not arbitrary; it’s influenced by compelling clinical evidence and the quest for improved patient outcomes.
Clinical Evidence: The Backbone of Change
Several studies have highlighted the benefits of spinal blocks over general anesthesia in joint replacement surgeries. For instance, research published in the British Journal of Anesthesia noted that patients who received spinal blocks experienced quicker recovery times compared to those who underwent general anesthesia1. This speedier recovery can significantly reduce hospital stay durations, leading to cost savings for both the patient and the healthcare facility.
Another study found that spinal anesthesia was associated with less blood loss during total hip arthroplasty, further enhancing patient safety and reducing potential complications.
Spinal Block vs. General Anesthesia with The Epidural Positioning Device
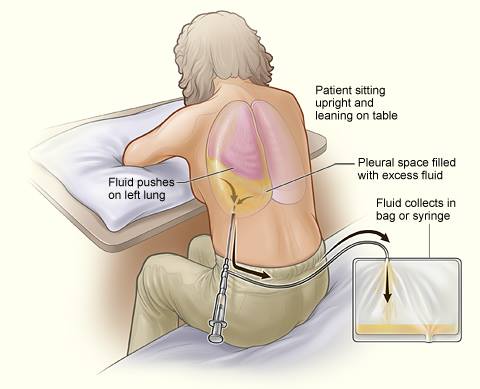
The primary difference between a spinal block and general anesthesia lies in the area of the body that is numbed for the surgery. While general anesthesia renders the patient unconscious and unable to feel pain throughout the entire body, a spinal block specifically numbs the lower half of the body while the patient remains conscious.
This localized approach offers several advantages. First, it eliminates the risks associated with general anesthesia, such as postoperative nausea, vomiting, and cognitive dysfunction. Second, spinal blocks allow for faster recovery times, as patients do not need to regain consciousness post-surgery. Finally, spinal blocks can provide effective postoperative pain relief, reducing the need for opioid analgesics and their associated side effects.
The increasing preference for spinal blocks in joint replacement surgeries is not a passing trend but a well-founded approach backed by clinical evidence. By opting for spinal blocks, surgeons are choosing a path that promises better patient outcomes, improved surgical efficiency, and enhanced patient safety. So how can we support this trend and improve staff safety?
The Pivotal Role of the Epidural Positioning Device in Surgery Departments
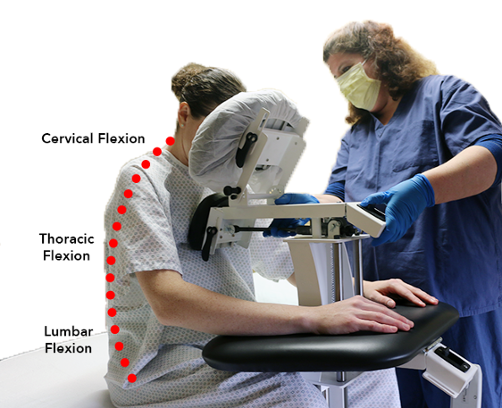
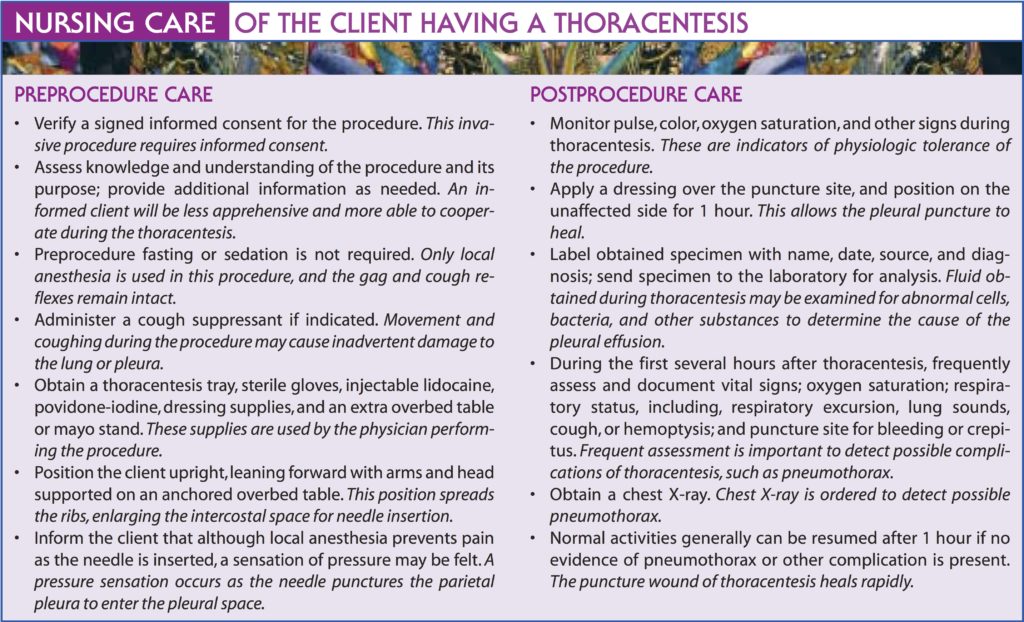
The EPD plays a vital role in surgery departments where spinal blocks are routinely performed. Its key function is to facilitate accurate patient positioning, which is crucial for the successful administration of a spinal block. By ensuring optimal positioning, the EPD significantly enhances patient safety, reducing the risk of complications associated with spinal block administration.
The Undeniable Benefits of the EPD in Surgery
The advantages of using the EPD extend beyond patient safety. From a healthcare provider’s perspective, it introduces improved ergonomics into the surgical environment. The device’s design reduces physical strain on nurses, doctors, and other surgical staff, thus preventing work-related injuries and promoting a healthier work environment.
Moreover, the Epidural Positioning Device contributes to improved safety and efficiency for surgical staff. By enabling precise positioning, it minimizes the risk of complications, saving valuable time in the operating room and leading to more effective surgical procedures.
Backing Claims with Evidence: Case Studies and Statistics
The efficacy of the EPD is not just a claim; it’s a fact underscored by real-world examples and solid data. Numerous surgery departments across the nation have reported enhanced patient outcomes and operational efficiency after incorporating the EPD into their spinal block procedures.
A Resounding Call to Action
In light of these compelling benefits, the conclusion is unequivocal: the EPD is an indispensable asset for any surgery department performing spinal blocks. Its contribution to patient safety, improved ergonomics for healthcare providers, and overall operational efficiency make it a must-have tool. We at SPH Medical urge all hospitals to consider its implementation. With the Epidural Positioning Device, embrace a new standard of care that promises exceptional benefits for patients and healthcare providers alike.