Epidural Pain Relief and patient positioning occurs in both the hospital and outpatient settings. Epidurals are regional pain analgesics commonly administered before intense pain during labor, surgical procedures, or for chronic pain in the back and neck. Epidural anesthesia blocks pain in an area of the body. Epidurals provide labor pain relief rather than anesthesia, which is total lack of feeling. Proper patient positioning is important to ensure the correct location for the epidural placement but ensuring healthcare worker safety is equally important.
Epidural steroid injections (ESIs) are a treatment for lower back pain and leg pain. For decades, ESIs have been considered a central component of nonsurgical approaches to sciatica and lower back pain. Epidurals and epidural steroid injections involve injecting a local anesthetic (and a steroid medication in the case of ESIs) directly into the epidural space that surrounds the spinal cord and nerve roots.
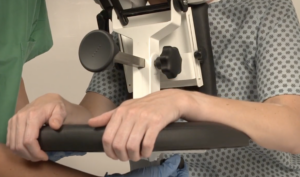
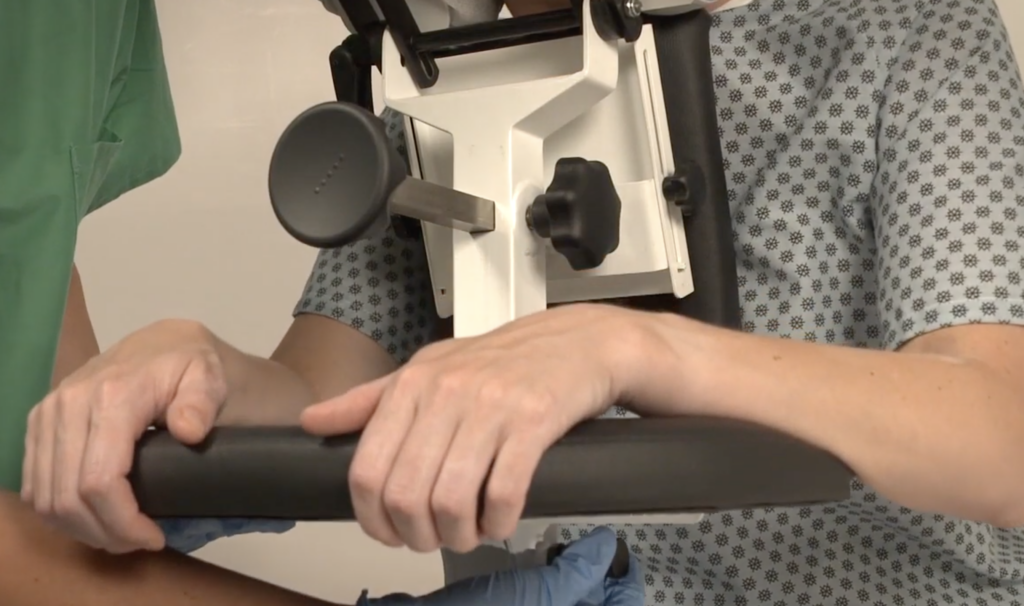
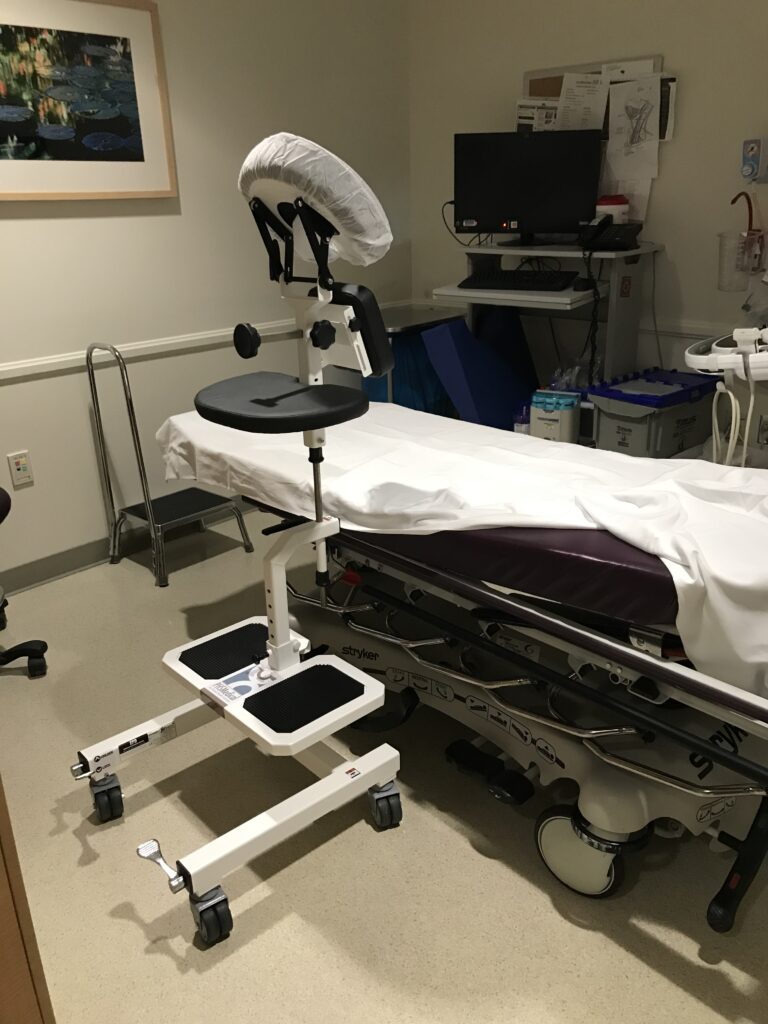
Today, much emphasis is placed on the positioning of the patient for receiving epidural pain relief for reasons of safety, for both the patient and the medical staff. Being able to quickly and comfortably administer an epidural decreases risks to all involved. To aid in this, the epidural positioning chair (EPD), commonly known as the epidural positioning device (EPD), or epidural chair, has become a valuable piece of equipment. The EPC is used in labor and delivery departments and in surgical areas to position the patient properly for the epidural procedure. The mobile positioning chair is lightweight, easy to move, and locks into place to allow for easier and safer administration of epidural pain relief.
Epidural Pain Relief, Positioning a Patient
Making sure a patient is in the right position can sometimes prove difficult. For instance, a patient’s range of motion may be limited because of pregnancy or injury. A patient’s level of distraction because of pain may also impede proper positioning administration of the epidural.
Positioning a patient for an epidural is an important consideration, as risks exist for the patient and for the medical staff administering the medicine. Throughout history, different positions have been used, and more recently, specific positions are used for specific bodily locations of epidural administration.

The various positions used usually depend on the condition of the patient. Pregnant women, for instance, are often put into a Sims position (left lateral decubitus, left leg straight, right leg bent), but it may be done with the patient sitting with their back arched, often described as an “angry cat” or “boiled shrimp” position. An epidural chair makes properly positioning patients very simple.
Epidural Pain Relief Injection and Risks to the Patient
For the patient, risks include low blood pressure in 10-20% of patients. There is a 1% risk of intravascular injection, puncture in spinal cord, and failure to block. There is less than 1% risk of infection, headache, bleeding, and allergic reaction. Patients are monitored closely during and after epidural placement, especially delivering. As mentioned, administering an epidural safely and comfortably is of utmost importance in reducing risk, and the EPD has come to play a significant role in this.
Healthcare Worker Safety
Providing epidural pain relief has improved healthcare worker safety as well. Often, a professional (or multiple professionals) are holding a patient in place manually. Pain during labor or from injury may cause a patient to unexpectedly move while receiving an epidural. Or, having an adverse reaction to the epidural may cause the patient to move. Any patient motion requires staff reaction and counter, creating musculoskeletal strain for the professional. The pushing, pulling, tugging, lifting and catching required of the healthcare worker can lead to strain injury instantaneously or over time. Very often, healthcare workers use nearby non-medical equipment like stools chairs and tables when trying to make the patient ready and as comfortable as possible for the injection. These stools, tables, and chairs often have rollers, which then require the healthcare worker to counter any movement with adverse pressure or motion. The necessity of this practice, and the risk of injury that comes with it, while being in common practical use all over the world, has been all but eliminated with the EPD or Epidural Chair. Using the EPD eliminates the physical strain on the professional, thereby eliminating much of the risk to healthcare workers associated with administration of epidurals.
Having the patient in the correct position with an epidural positioning device makes quick and safe epidural administration possible with fewer staff members. By reducing manual patient handling the EPD is a simple yet highly effective device that reduces risks for both patients and healthcare staff.