Environmental Disinfection To Prevent Hospital Acquired Infections (HAI’s)
Hospital Acquired Infections (HAI’s) are a common cause of death in healthcare facilities and represent a significant cost burden. A recent study found that influenza-associated hospitalization affected 156,097 people in Germany. However, many of these infections could be prevented by proper cleaning and disinfection of the environments in which they occur. Hospitals are challenged with having sick patients that come in from the community with transmittable diseases that can often put other patients at risk. In other cases like patients who develop Clostridium Difficile infections while in the hospital can also transmit this very difficult to kill, spore forming bacteria, to nurses, objects, or surfaces where the spores can survive for months. For this reason a focus on environmental disinfection of patient care areas and surgical suites is absolutely critical.
Top Stubborn Pathogens That Cause Hospital Acquired Infections
Several resistant organisms cause significant problems in healthcare facilities. The CDC has identified the following as the most common multidrug-resistant healthcare-associated pathogens:
- MRSA
- Clostridium deficile
- CRE
- Pseudomonas aeruginosa
- Norovirus
What Are The 5 Common Challenges Facing Healthcare Facilities In Environmental Disinfection?
Unfavorable Structural Design
Two central issues facing healthcare facilities are the design of their physical plant and the limitations that these restrictions imposed on the disinfection process. Structurally, healthcare facilities are often built with materials that inhibit disinfection. The most common example is the glazed tile, often used in hospitals to protect against infection. This surface is difficult to disinfect and can also harbor organisms.
Overcrowded Hospital Units
Another challenge facing healthcare facilities is the overcrowding of patients. This increases the number of patients in beds, chairs, and others, leading to further contact with surfaces in the patient’s environment. It also leads to more cross-contamination of surfaces as staff must frequently change linens or clean bedding on these beds.
Poor Toilet Sanitation
Toilets present a significant challenge because of poor sanitation and maintenance. The CDC reports a significant number of inpatient facilities have poorly sanitized toilets. Contamination of these surfaces can be spread between patients and other areas in the facility.
Misuse Of Handwash Sinks
Handwashing stations are in important tool in fighting infections and cross contamination. However they can also be are a central focus of environmental contamination in healthcare facilities. There can be a significant amount of bacterial contamination that occurs on these sinks. Therefore, cross-contamination is risky between areas without proper cleaning and disinfection.
Hospital Waste Management
Finally, hospital waste management presents particular risks to environmental hygiene. Healthcare facilities dispose of their used items in many ways. The inappropriate handling of these items can lead to toxic pathogens, which may be dangerous to patients.
What Are The CDC Guidelines For Hospital Disinfection?
Infection control in hospitals is critical to preventing organisms from infecting patients. This includes the disinfection of surfaces touched by the hands or clothing of healthcare personnel, patients, or visitors to prevent disease transmission.
There are guidelines developed by the federal government and the CDC which require hospitals to disinfect their patient rooms after each day. The guidelines state that room surfaces, such as floors, walls, and toilets, should be disinfected with a recommended detergent solution every 24 hours. Additionally, healthcare facilities should perform surface disinfection of rooms where patients change linens or bedding frequently.
How Do You Perform Disinfection?
The CDC guidelines recommend that healthcare facilities disinfect their patient rooms using a multi‐component, antimicrobial system to remove bacteria resistant to antibiotics that can cause infection. The recommended EPA approved product for these surfaces is Oxydiff.
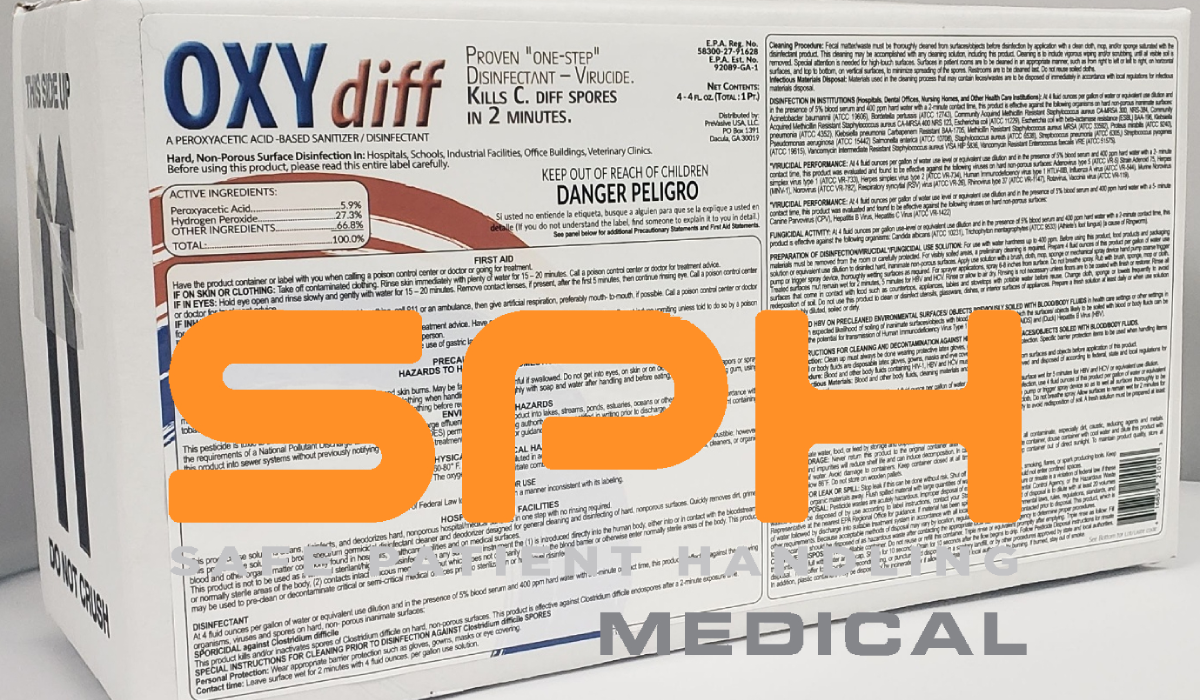
Why Use Oxydiff?
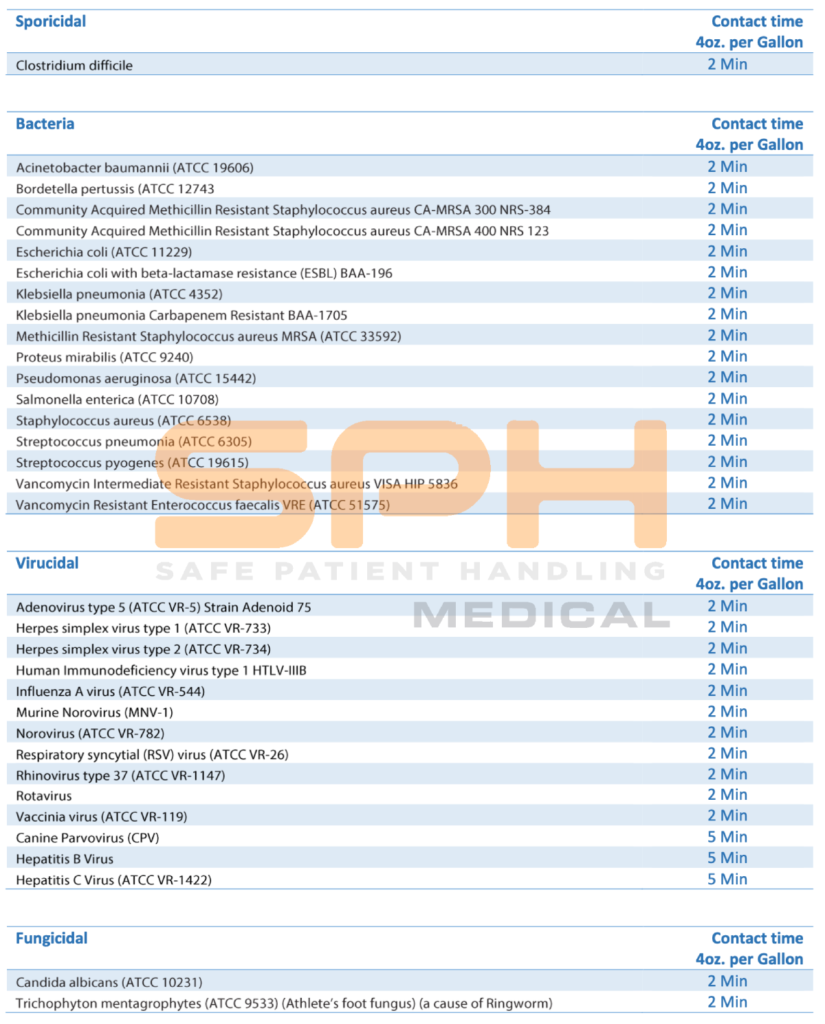
The chemical solution is a broad-spectrum disinfection EPA approved to kill C. diff spores in 2 minutes and an extremely wide range of other organisms, including viruses, fungi, and molds. The solution is also non-corrosive and is rinse-free after application. It allows for efficient disinfection because it is easy to apply with a sprayer, mop, or cloth. It costs about the same as other disinfectants but may be cheaper because its ease of application reduces personnel labor time.
Why Is Environmental Disinfection Critical To The Success Of Hospital Acquired Infections Prevention?
Environmental disinfection is critical to the success of Hospital Acquired Infections prevention because it reduces the overall cross-contamination within a given facility and thereby helps prevent the transmission of infectious organisms in healthcare facilities. In addition, it is also critical because it contributes to a cleaner environment and better patient health outcomes.
Hospital Acquired Infections Prevention Conclusion
Hospital Acquired infections are costly to hospitals and healthcare systems because they negatively impact patient care, patient satisfaction, staff turnover, and device failure rates. Hospitals must prioritize environmental disinfection in light of rising costs and potential loss associated with HAIs.