Although there are cases where a patient leaving bed is not possible for a variety of reasons, in the majority of cases, encouraging a patient to become mobile is beneficial. Early and progressive mobility essentials are beneficial for both the patient’s physical healing and mental well-being.
Getting patients out of bed early in the healing process reduces:
- The length of time a patient must be mechanically ventilated
- The overall length of stay in the intensive-care unit
- Short-term complications
- Long-term physical and mental disabilities
Patients also won’t need as many sedatives when they ambulate, and any sedatives they need, for whatever reason, will not be at high dosages. Too, helping a patient be mobile is a bonding process between not only the patient and the staff but also between staff members, which can only improve the level of care. Such improvement is not limited to that of the patient in question, either, as the bonding between the various staff members will affect every patient who is under their care.
In 2015, the Journal of the American Medical Association Internal Medicine published Hodgson et al., a study on the positive impact of early mobility on elderly patients who had been mechanically ventilated. The mobilized patients exhibited higher scores on the Medical Research Council Dyspnea Scale than those who were not mobile. They also lived longer post-discharge than those who could not become mobile.
Some other evidence based benefits of early mobility on patients after discharge include the following:
- More than a third of patients avoided ICU-Acquired Weakness.
- If a patient experienced ICU-Acquired Delirium, the duration of such delirium was 50% shorter than in those patients who were not mobile.
- Patients required 10% less time on a ventilator.
- More than 50% of patients were independently functional post-discharge.
- One in eight patients who would have otherwise died survived.
Progressive Mobility Essentials For New Patient Mobility Strategies
Aside from the multidisciplinary approach, there are other strategies for hospital staff regarding early patient mobility. They must assess each patient individually and realize that not every patient will be able to be mobile. Even if a patient cannot get out of bed, for example, there are things that the patient can do with a nurse or physical therapist while remaining in bed. Exercises, turning to different positions to avoid bedsores, and just sitting up can work wonders.
Safety is also obviously a concern. A patient might be willing, but the parameters of the case might make it impossible for the person to be safely mobile. Also, even though you might adopt general safety criteria, each case requires well-reasoned decision making regarding mobility. This highlights the great strength of the multidisciplinary strategy. Throughout the team, there will be enough experience and expertise to make the right decisions regarding early patient mobility.
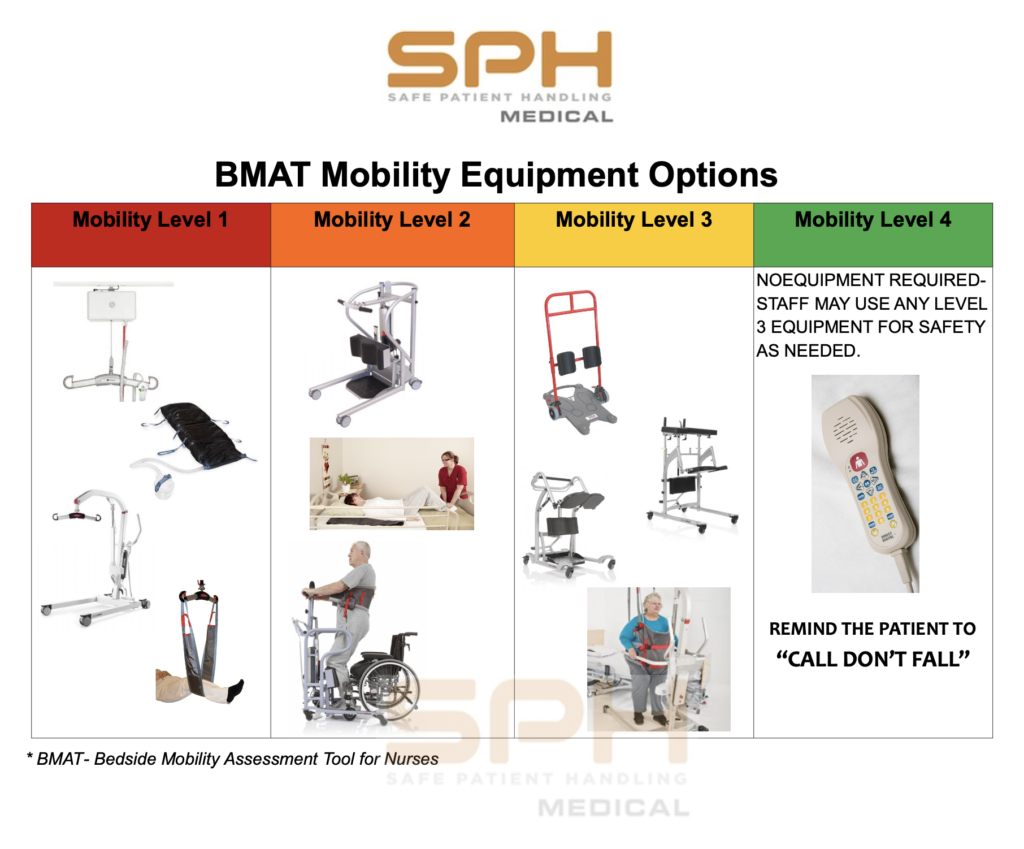
The Banner Mobility Assessment Tool, or BMAT, as is is now known, is a common tool that is used to asses the mobility level of a patient by going through some simple functional tests. The test are fairly simple but yield validated results. The nurse will have the patient sit and shake, stretch and point, stand, then walk. After going through the BMAT assessment the patient is given a BMAT level, 1, 2, 3, or 4. If after the level 3 standing test the patient can bear weight but if any assistive device (cane, walker, crutches) is needed, patient is determined to be Mobility Level 3, and the appropriate assistive tool should be selected. A validated Nursing mobility assessment is often the cornerstone of a sustainable program. As part of California’s AB1136 (CA LC 6403.5) legislative requirements, a validated patient mobility assessment tool provides valuable documentation about patient mobility status and communication between staff.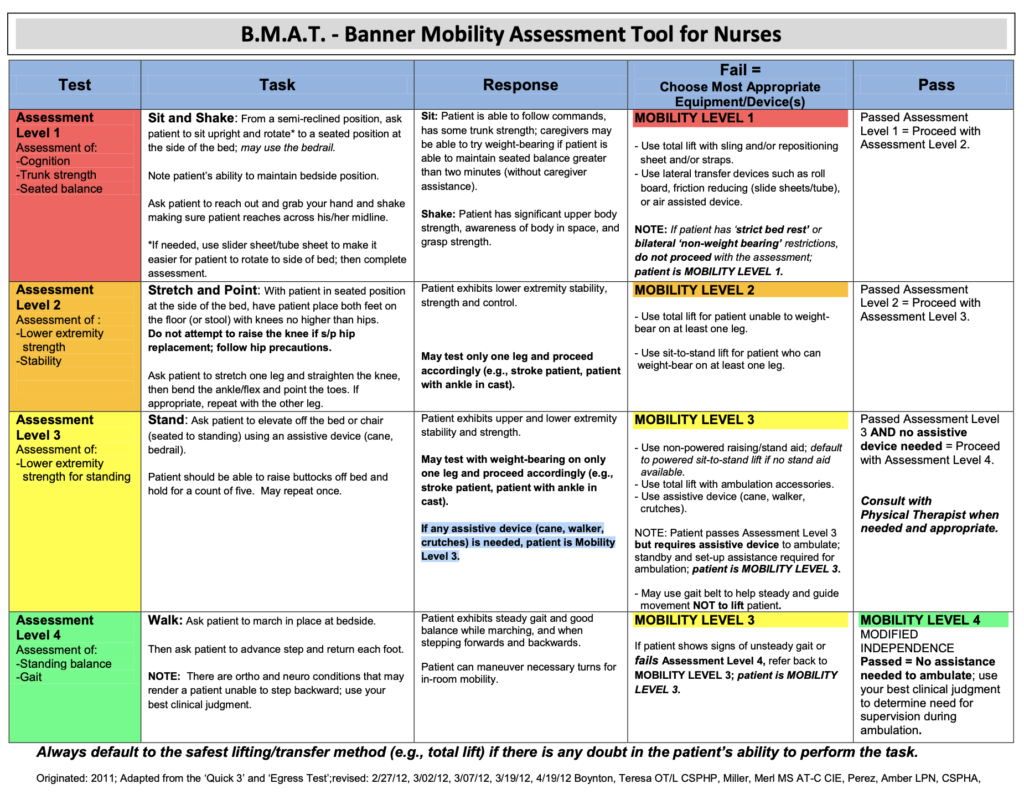
The RoWalker for Early and Progressive Mobility Essentials
After assessing the patients’ mobility level, one of the best ways to get a patient up and moving as part of a safe patient handling program is to use a sturdy and stable platform walker, such as the SPH Medical RoWalker. This kind of walker is the best choice because it has wheels with directional casters and brakes on the wheels. With these features,
the nurse or therapist can safely get a patient standing at bedside with the brakes on, or walk the length of a hallway without drifting from side to side, a key benefit of the directional casters.
Additionally, having a rolling walker with the proper attachments makes it a snap to attach IV bags, various monitors, and even an oxygen tank to it. That way, the patient can get all the benefits of mobility without having to leave vital devices behind. A SPH Medical RoWalker also has a basket attached to the front so that some of this critical care equipment can go with the patient as they progress, move further away from bedside, and take steps towards recovery.
References:
https://www.ahrq.gov/hai/tools/mvp/modules/technical/intro-early-mobility-fac-guide.html
https://www.medtronic.com/covidien/en-us/clinical-solutions/icu-early-mobility/about.html
https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03741-z